Translate this page into:
Red forehead dot(s) and migraine
2 Department of Pathology, School of Medicine, Acibadem Mehmet Ali Aydinlar University, İstanbul, Turkey
Correspondence Address:
Emel �zt�rk Durmaz
Acibadem Maslak Hospital, Büyükdere Caddesi 40, Maslak 34457, Istanbul
Turkey
| How to cite this article: Durmaz E�, Demirkesen C. Red forehead dot(s) and migraine. Indian J Dermatol Venereol Leprol 2020;86:704-705 |
Sir,
Migraine headaches are characterized by recurrent unilateral or bilateral pain progressively increasing in intensity and commonly accompanied by other symptoms including nausea, vomiting, dizziness, photophobia or phonophobia.[1],[2] Migraine with cutaneous stigmata is an extremely rare phenomenon.[2]
A 36-year-old male patient presented with a 3-day history of tender, red-coloured skin lesions on the forehead that had appeared during a severe migraine attack. He did not give a history of massaging the area or applying heat or cold pads on this area. He had suffered several migraine attacks within the past 3 months and had noted these red spots during each episode of migraine and interestingly, these spots used to disappear with the resolution of migraine. His family history was unremarkable. He was taking sertraline for the past 5 years, liraglutide since one month and mefenamic acid occasionally (to control his headache) since 3 months. On dermatologic examination, there were several ovoid and triangular, erythematous and telangiectatic macules on the forehead and along the hairline [Figure - 1]. Dermatoscopy revealed vessels in clods on an erythematous background, which faded on applying pressure [Figure - 2]. His neurologic examination was normal and laboratory tests for sexually transmitted diseases, rheumatoid factor and antinuclear antibodies were negative. Initial clinical differential diagnoses were connective tissue disease (CREST syndrome), fixed drug eruption and cutaneous angiosarcoma. Histopathologic examination of a punch biopsy specimen showed a perivascular dermatitis with abundant plasma cells and extravasated erythrocytes. In addition, vascular changes, such as the presence of fibrinoid material within the vessel walls and endothelial swelling, were evident [Figure - 3]. The lesions had completely disappeared within one week, along with the resolution of the migraine attack.
 |
| Figure 1: Red forehead dots during a migraine attack, variable in size and shape |
 |
| Figure 2: Dermatoscopy showing vessels in clods on an erythematous background (Dermlite DL3N PigmentBoost®; ×10; non-polarized) |
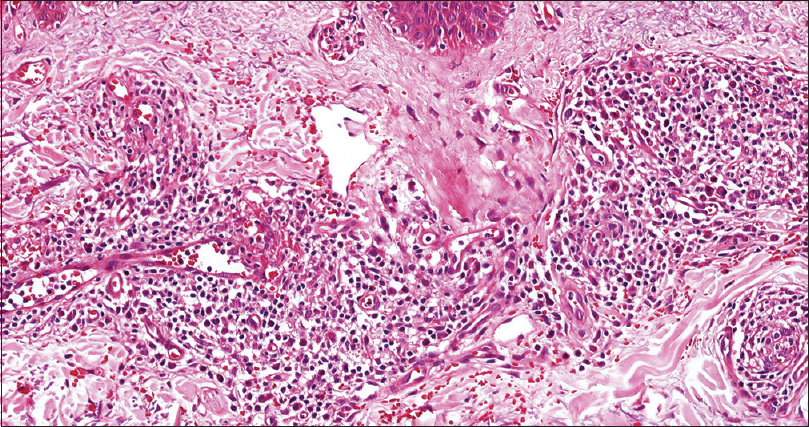 |
| Figure 3: Perivascular dermatitis, with abundant plasma cells and extravasated erythrocytes in the upper dermis. Fibrinoid material is present in a focal area at the vessel wall (H and E, ×200) |
There are several cutaneous disorders characterized by facial erythema, burning pain and increased temperature in association with headache syndromes. Among these are erythermalgia of the face (a variant of erythromelalgia), red ear syndrome and red forehead dot syndrome.[1] Red forehead dot/spot/mark during recurrent migraine attacks is a recently described novel phenomenon. Red forehead dot syndrome more commonly escorts severe migraine attacks.[1] The size and number of red dots are also usually correlated with the intensity of migraine.[1],[2] The red dots may extend from the forehead to the periorbital area in the classic V1 distribution of the trigeminal nerve.[1] Along with the red forehead mark, there may be profuse sweating and periorbital ecchymosis as well.[1],[2],[3],[4] Although originally described as a ping-pong ball-like discoid forehead mark, linear or band-like marks on the forehead and nose have also been reported.[2] In our case, the red spots were of variable sizes and shapes (triangular and ovoid). As in our case, the markings have been noted to last for a few days and then spontaneously resolve.[2]
Owing to the rarity of the 'red forehead dot syndrome', definitive treatment of this phenomenon is unknown. It is reasonable to direct treatment at the underlying migraine. As in red ear syndrome, lifestyle modification and avoidance of migraine triggers may reduce the frequency of attacks. Theoretically, botulinum toxin type A, which is effective in rosacea and red ear syndrome, may reduce erythema and alleviate burning pain of red forehead dot syndrome.[5]
The pathophysiology of migraine-associated red forehead dot syndrome is an enigma, yet two theories have been proposed.[1],[3],[4] One theory describes definitive trigeminovascular system activation during a migraine attack. According to this theory, primary aberrant activation of the trigeminovascular system in headache syndromes precedes the release of vasoactive peptides such as nitric oxide, calcitonin gene-related peptide and substance P, which are incriminated in the development of extracerebral vasodilatation. Another theory focuses on an autonomic nervous system dysfunction; i.e., trigemino-cervical autonomic reflex. According to this theory, the trigemino-cervical autonomic circuit, consisting of a brainstem connection between the trigeminal nerve and facial parasympathetic outflow is primarily over-activated in headache syndromes, resulting in extracerebral vasodilatation. In our opinion, cutaneous red patches during migraine do not reflect mere blood vessel dilatation, but concomitant inflammation as well. The presence of perivascular inflammatory changes within the biopsy sample in our case might support the former theory which considers vasodilatation in conjunction with inflammation of blood vessels.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Sethi PK, Sethi NK, Torgovnick J. Red forehead dot syndrome and migraine. J Headache Pain 2007;8:135-6.
[Google Scholar]
|
| 2. |
Berdouk S, Khan S. Migraine with extensive skin markings: A case report. Int J Emerg Med 2018;11:32.
[Google Scholar]
|
| 3. |
Sethi PK, Sethi NK, Torgovnick J. Teaching NeuroImages: Red forehead dot syndrome and migraine revisited. Neurology 2015;85:e28.
[Google Scholar]
|
| 4. |
Monaghan BM, Smyth S. Teaching NeuroImages: Red forehead dot syndrome and migraine revisited. Neurology 2016;86:697-8.
[Google Scholar]
|
| 5. |
Castellanos-Gonzalez M, De Manueles F, Martos MG, Rodríguez MAS. Successful treatment of red ear syndrome with botulinum toxin type A. Indian J Dermatol Venereol Leprol 2019;85:107-8.
[Google Scholar]
|
Fulltext Views
19,947
PDF downloads
782





