Translate this page into:
Prevalence of metabolic syndrome and cardiovascular changes in patients with chronic plaque psoriasis and their correlation with disease severity: A hospital-based cross-sectional study
2 Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi, India
3 Department of Endocrinology and Metabolism, All India Institute of Medical Sciences, New Delhi, India
4 Department of Cardiology, All India Institute of Medical Sciences, New Delhi, India
5 Department of Cardiac Radiology, All India Institute of Medical Sciences, New Delhi, India
6 Department of Bio-statistics, All India Institute of Medical Sciences, New Delhi, India
Correspondence Address:
Neena Khanna
Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi
India
| How to cite this article: Kothiwala SK, Khanna N, Tandon N, Naik N, Sharma VK, Sharma S, Sreenivas V. Prevalence of metabolic syndrome and cardiovascular changes in patients with chronic plaque psoriasis and their correlation with disease severity: A hospital-based cross-sectional study. Indian J Dermatol Venereol Leprol 2016;82:510-518 |
Abstract
Background: Previous epidemiological studies suggest an association between psoriasis and metabolic syndrome and risk of subclinical atherosclerosis. However, there is a paucity of data in the Indian population on these associations. Objectives: To evaluate the prevalence of metabolic syndrome and subclinical atherosclerosis in patients with chronic plaque psoriasis compared to healthy controls and to correlate the prevalence of metabolic syndrome with severity of psoriasis. Methods: A hospital-based cross-sectional study was performed on 140 patients with chronic plaque psoriasis and 140 controls. Psoriasis was categorized as mild, moderate and severe based on psoriasis area and severity index (<10, 10–14 and ≥15, respectively) and as disease of short (<1 year), intermediate (1–3 years) and long duration (>3 years). In all patients and controls, body mass index was calculated, blood pressure and waist circumference were measured and fasting bloaod sugar and lipid profile were estimated. Metabolic syndrome was diagnosed by the presence of 3 or more of the modified National Cholesterol Education Program's Adult Treatment Panel III criteria. A subset of 30 psoriatic patients and 30 healthy controls were selected by the systematic sampling method for cardiac evaluation including electrocardiography, echocardiography and carotid intima-media thickness measurement. Results: The prevalence of metabolic syndrome was significantly more in psoriatic patients than in controls (39.3% vs. 17.1%, odds ratio = 3.13). Psoriatic patients also had a significantly higher prevalence of hypertension, abdominal obesity and diabetes. There was a significant trend to increase in prevalence of metabolic syndrome, hypertension and type 2 diabetes with increased severity and longer duration of the psoriasis. Patients with psoriasis had significantly higher carotid intima-media thickness (mean 0.61 mm ± 0.01 mm vs. 0.37 mm ± 0.01 mm) than controls. Limitation: This was a hospital-based cross-sectional study with a relatively small sample size. A prospective study with a larger sample would have validated the results further. Conclusion: There is a significantly higher prevalence of metabolic syndrome in psoriasis patients as compared to controls; the prevalence of metabolic syndrome and its components increases with severity and duration of psoriasis. There is a higher prevalence of subclinical atherosclerosis in patients with psoriasis thus increasing the risk of cardiovascular disease. We suggest that patients with moderate to severe psoriasis be screened routinely for metabolic syndrome and cardiovascular disease and encouraged to correct modifiable cardiovascular risk factors.Introduction
Psoriasis is a chronic, systemic, inflammatory disease with several clinical variants, the most common being chronic plaque psoriasis. It affects 1–3% of the population worldwide.[1] Despite the fact that psoriasis carries minimal risk of mortality, it is associated with significant morbidity which may have a significant impact on quality of life of patients even if a relatively limited body surface area is involved.[2] Globally, psoriasis has been reported to be associated with metabolic syndrome including obesity, dyslipidemia, diabetes, hypertension and more recently, atherosclerosis.[3],[4],[5],[6] However, most of these associations are based on computerized medical databases. Despite evidence suggesting that Indians are genetically and environmentally more susceptible to develop metabolic syndrome, there is a paucity of data on the association between psoriasis and metabolic syndrome from the Indian subcontinent.[7],[8],[9],[10],[11],[12] Our objective was to evaluate the prevalence of metabolic syndrome in patients of chronic plaque psoriasis compared to healthy controls and to correlate the prevalence of metabolic syndrome with severity and duration of psoriasis. We also evaluated the prevalence of cardiac changes and subatherosclerosis in cases and controls selected from the original cohort.
Methods
This cross-sectional study was conducted at All India Institute of Medical Sciences, New Delhi between January 2011 and October 2012, after receiving ethical clearance from the Institute's ethical board.
Sample size was calculated using the following data: from the available information, it was expected that 30% of patients with psoriasis would have metabolic syndrome.[7],[10] The required sample size for an error margin of 8% and confidence level of 95% was 140. Consecutive patients with chronic plaque psoriasis attending the dermatology outpatient department were recruited after obtaining written informed consent. We included patients who were 18 years or older and excluded patients who had taken systemic therapy for psoriasis including acitretin, cyclosporine, methotrexate, phototherapy or biologics in the 2 months before their enrollment. After taking informed consent, healthy controls of similar age and sex were chosen from the general population including colleagues, hospital staff and relatives or attendants of dermatology inpatients. From this original cohort, 30 patients and 30 controls were selected by the systemic sampling method to study the prevalence of cardiac changes and subclinical atherosclerosis.
The study groups were evaluated by a dermatologist who recorded their demographic, biometric and the other relevant data, including age, sex, weight, height, body mass index, waist circumference, blood pressure, smoking and alcohol consumption habits, duration of disease, type and severity of psoriasis, presence and distribution of psoriatic arthropathy and concomitant medications. Smokers and alcohol drinkers were classified into current and ex-smokers or alcohol drinkers. Current smokers were defined as persons smoking tobacco at the time of study and those who stopped smoking less than 6 months ago. Ex-smokers were those who had stopped smoking more than 6 months before enrollment in the study. Non-smokers were persons who had never smoked a tobacco product. Similarly, current alcohol drinkers were defined as those who continued to have alcoholic beverages at the time of study and those who had stopped alcohol intake for less than 6 months. Ex-drinkers were defined as those who had not consumed alcohol for more than 6 months before enrollment. Non-drinkers were persons who had never consumed alcoholic drinks.
Psoriasis was classified as of short (<1 year), intermediate (1–3 years) or long (>3 years) duration. Patients were classified as having mild, moderate or severe psoriasis based on the psoriasis area and severity index (PASI) score (<10, 10-14 and >14 respectively). Body mass index was calculated as the ratio of weight in kg to the square of height in m 2. Waist circumference was measured by locating the uppermost part of the hip bone and placing a measuring tape around the abdomen snugly but without causing compression of the skin, ensuring that the tape was horizontal. Blood pressure was recorded as an average of two measurements, taken 5 min apart after subjects had been at rest for at least 10 min. A venous blood sample was taken in all patients and controls, after overnight fasting (at least 8 h) to estimate the fasting blood sugar (enzymatic method) and fasting lipid profile (enzymatic method).
The diagnosis of metabolic syndrome was made based on the presence of ≥3 criteria of the modified National Cholesterol Education Program's Adult Treatment Panel III:[13] waist circumference >102 cm in men or >88 cm in women, hypertriglyceridemia ≥150 mg/dL, high-density lipoprotein cholesterol <40 mg/dL in men or <50 mg/dL in women, blood pressure ≥130/ 85 mmHg and fasting plasma glucose ≥100 mg/dL.
Thirty patients and 30 controls were then selected for evaluating the prevalence of subatherosclerosis and cardiac changes. Cardiac changes were studied with electrocardiography and echocardiography by a cardiologist. Carotid intima-media thickness (CIMT) of both common carotid arteries was measured by a cardiovascular radiologist using a high-resolution B-mode ultrasound (ATL 3500) with the 5–10 MHz linear array broadband transducer positioned in the common carotid artery, 1 cm distal to the carotid bifurcation in the posterior wall. Scanning involved examination of the common carotid artery both in longitudinal and transverse planes [Figure - 1].
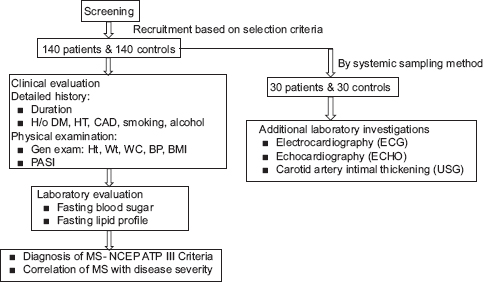 |
| Figure 1: Flowchart of the study. DM: diabetes mellitus, HT: hypertensions CAD: coronary artery disease, Ht: height, Wt: weight, WC: waist circumference, BP:blood pressure, BMI: body mass index, PASI: psoriasis area severity index, MS: metabolic symdrome, NCEPATPIII: national cholesterol education program's adult treatment panel III |
Statistical analysis
Data analysis was done using Stata software version 11.1 (StataCorp. 2009, College Station, TX: StataCorp LP). Quantitative characteristics such as age, waist circumference, systolic and diastolic blood pressures, high-density lipoprotein and triglyceride levels were compared between patients and controls using a two-sample t-test. Wilcoxon rank-sum (Mann–Whitney) test was also used for non-normally distributed values such as carotid intima-media thickness. Qualitative variables such as sex, duration and severity classifications of disease, smoking and alcohol use were compared between patients and controls using Chi-square test. The prevalence of metabolic syndrome and its components in patients with chronic plaque psoriasis of different severities and durations was compared using a trend Chi-square test. The prevalence of metabolic syndrome among patients was calculated as a proportion along with a 95% confidence interval. Odds ratios with 95% confidence intervals were calculated for different exposures using logistic regression analysis. Multiple logistic regression was employed to adjust for possible confounders. The correlation of different study parameters with severity of psoriasis was assessed by one-way ANOVA followed by Bonferroni correction for multiple comparisons. Odds ratio was also calculated along with 95% confidence intervals after categorizing study variables. A P< 0.05 was considered to be statistically significant.
Results
Demographic characteristics of the study population and disease characteristics are reported in [Table - 1]. Cases and controls were residents of various states of Northern India. The duration of psoriasis in our patients ranged from 3 months to 35 years while the psoriasis area and severity index (PASI) score of the 140 patients with psoriasis ranged from 2 to 30.
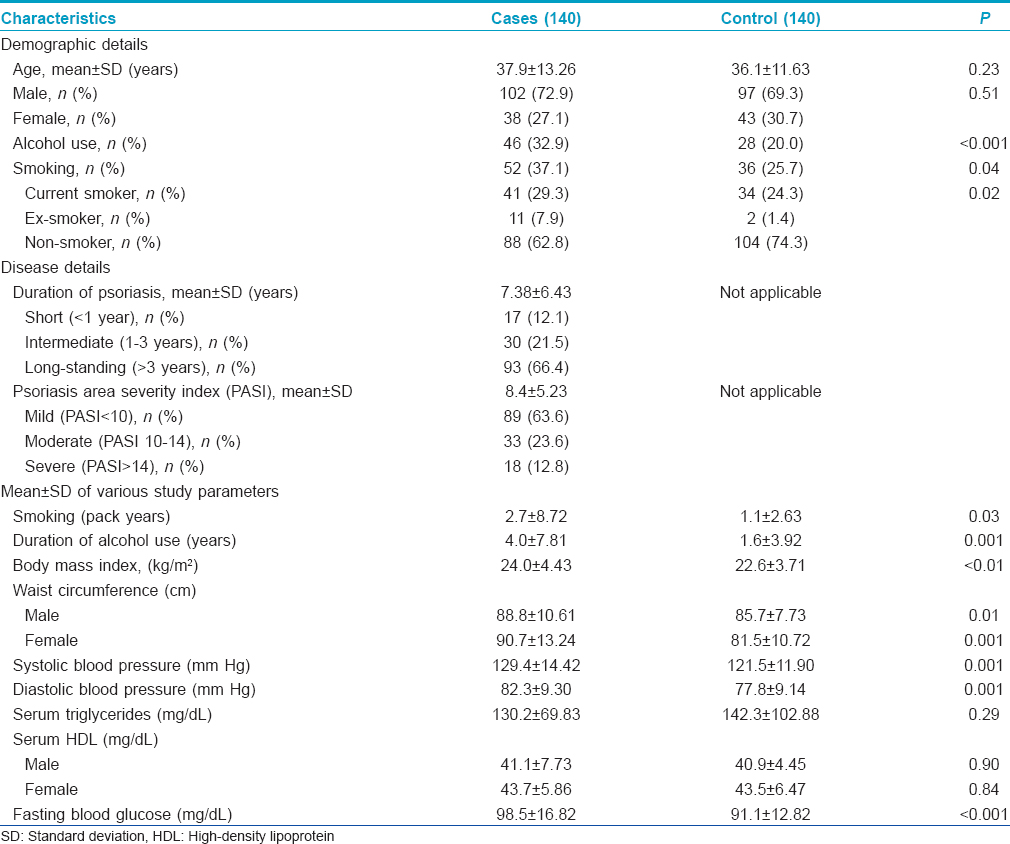
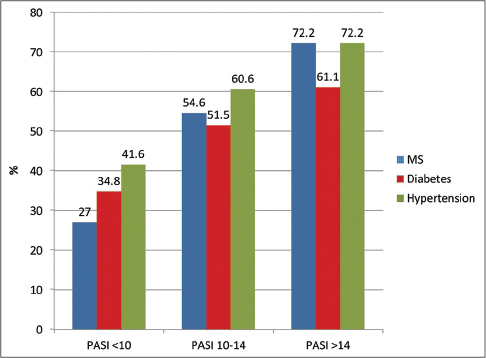
Based on modified National Cholesterol Education Program's Adult Treatment Panel III criteria, metabolic syndrome was diagnosed in 55 (39.3%) patients with chronic plaque psoriasis and 24 (17.1%) healthy controls. This difference was statistically highly significant (P< 0.001) with an odds ratio of 3.13 with 95% confidence interval 1.80–5.45 (P = 0.01). This association persisted even after adjusting for differences in age, gender, body mass index, smoking and alcohol use with the adjusted odds ratio being 2.50 with 95% confidence interval 1.34–4.67 (P< 0.01) [Table - 2]a. Adoption of the South Asia Modified cutoffs for abdominal obesity (≥90 cm for males and ≥80 cm for females) did not change the results overall (P< 0.001). The prevalence of metabolic syndrome in cases was then 59/140 (42.1%) and 30/140 (21.4%) in controls with an odds ratio of 2.67 (1.58–4.51) and adjusted odds ratio of 2.10 (1.15–3.82).
On studying the components of the metabolic syndrome, the following were found to be more common in psoriasis patients than in controls: central obesity in 26.4% versus 11.4% (odds ratio = 2.8, confidence interval 1.46–5.29), hypertension in 50.0% versus 29.3% (odds ratio = 2.4, confidence interval 1.47–3.95) and type 2 diabetes mellitus in 42.1% versus 21.4% (odds ratio = 2.5, confidence interval 1.48–4.26) [Table - 2]a.
Correlation of prevalence of metabolic syndrome and its components with severity and duration of chronic plaque psoriasis
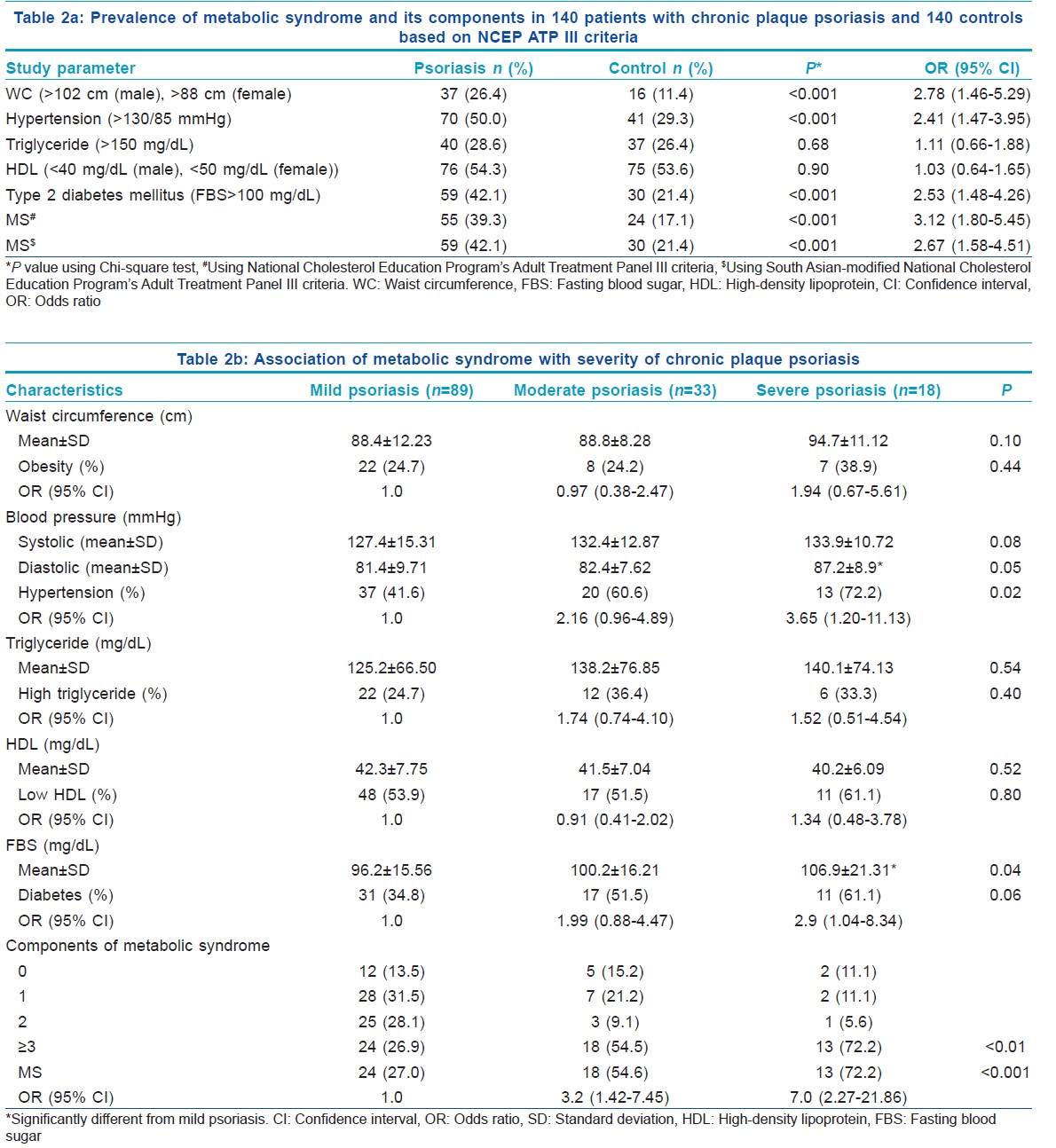
There was a linear trend of increase in the prevalence of metabolic syndrome with increasing severity of psoriasis in patients compared to controls (P< 0.001) and it remained statistically significant with odds ratio for metabolic syndrome being 3.2 (95% confidence interval, 1.41–7.45; P < 0.005) among patients with moderately severe psoriasis and 7.1 (95% confidence interval, 2.26–21.85; P < 0.001) among patients with severe psoriasis vis-a-vis patients with mild psoriasis [Table - 2]b. Patients with psoriasis of long duration had a higher prevalence of metabolic syndrome (52, 55.9%) when compared to those with disease of short and intermediate duration [11 (17.7%) and 3 (36.7%) respectively] There was also a statistically significant linear trend of increase in the prevalence of metabolic syndrome with increase in the duration of having had chronic plaque psoriasis (P = 0.04). As regards the association of components of metabolic syndrome with severity of psoriasis, patients with severe chronic plaque psoriasis had significantly higher prevalences of hypertension and diabetes than those with mild psoriasis [Table - 2]b and [Figure - 2]. We did not observe a significant difference in the prevalence of dyslipidemia between psoriasis patients and healthy controls.
 |
| Figure 2: Correlation of prevalence of metabolic syndrome (MS), hypertension and type 2 diabetes mellitus in 140 patients with chronic plaque psoriasis of different severities (PASI: Psoriasis area and severity index) |
Cardiovascular changes, subclinical atherosclerosis and chronic plaque psoriasis
Ten (33.3%) of 30 patients with chronic plaque psoriasis had abnormal findings on electrocardiography versus two (6.7%) of 30 controls, and the difference was statistically significant (P = 0.01, Chi-square test). The most common electrocardiographic abnormality was ST/T wave changes, present in 5 (16.6%) patients. On echocardiography, 7 (23.3%) of 30 patients with chronic plaque psoriasis had abnormal findings in contrast to 2 (6.7%) of 30 controls, but this difference was not statistically significant (P = 0.07, Chi-square test). The most common change on echocardiography was a low ejection fraction. One patient had both global ventricular hypertrophy and a low ejection fraction (50–55%). Going further, we compared cardiologic abnormalities among smokers and non-smokers in the patient group. Electrocardiographic abnormalities were noted in 45% of chronic plaque psoriasis patients who smoked as against 25% of non-smoker patients. Similarly, only 15% of non-smokers showed echocardiographic abnormalities compared to 36% of smokers amongst the patients of chronic plaque psoriasis.
Carotid intima-media thickness of the right common carotid artery in patients with chronic plaque psoriasis ranged from 0.4 to 1.2 mm with a mean of 0.7 mm ± 0.01 mm and median of 0.6 mm while in controls, it ranged from 0.3 to 0.6 mm with a mean of 0.4 mm ± 0.01 mm and median of 0.4 mm. Similarly, in the patients with chronic plaque psoriasis, the carotid intima-media thickness of the left common carotid artery ranged from 0.3 to 1.0 mm with a mean of 0.6 mm ± 0.01 mm and median of 0.6 mm while in controls, it ranged from 0.2 to 0.5 mm with a mean of 0.3 mm ± 0.01 mm and median of 0.3 mm. On applying the Student's t-test, carotid intima-media thickness of both the right and left common carotid arteries was found to be significantly higher in patients than in controls (P< 0.001) [Table - 3] and [Figure - 3]. One patient with psoriasis aged only 34 years had evidence of a soft plaque in the left common carotid artery near the carotid bulb causing a 30% stenosis [Figure - 4]. The same patient had sinus tachycardia on electrocardiography while the echocardiogram was normal. The duration of disease in this patient was 8 years and the psoriasis area and severity index (PASI) score was 18.
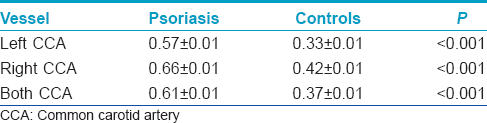
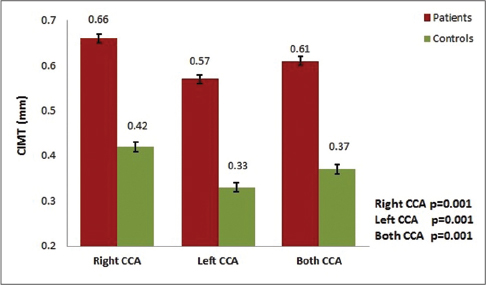 |
| Figure 3: Mean intima-media thickness of the right and left common carotid artery in 30 patients with chronic plaque psoriasis and 30 controls (CIMT: Carotid intima-media thickness, CCA: Common carotid artery) |
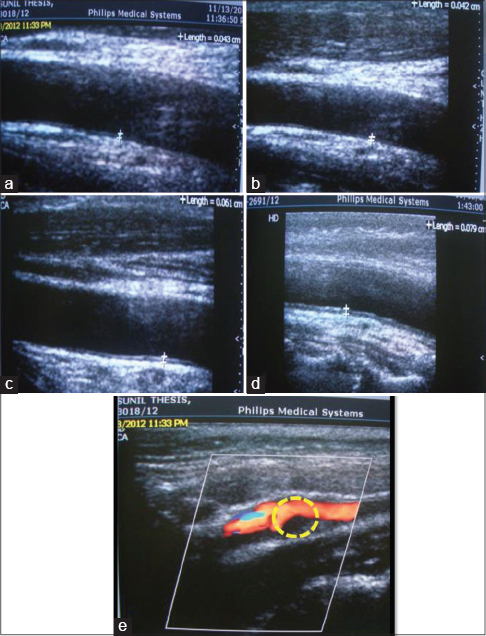 |
| Figure 4: B-mode ultrasonography showing normal carotid intima-media thickness in controls (a and b) and higher carotid intima-media thickness in patients with chronic plaque psoriasis (c and d). A soft plaque of size 3 mm × 8 mm in the left common carotid artery near the carotid bulb causing 30% stenosis of common carotid artery in a 34-year-old patient with chronic plaque psoriasis (e) |
Discussion
We found a linear increase in the occurrence of metabolic syndrome as the severity and duration of psoriasis increased. Though Gisondi et al. in a study of patients with psoriasis of longer than 6 months' duration observed an increased occurrence of metabolic syndrome in psoriasis patients, they did not find any correlation of metabolic syndrome with the severity of psoriasis.[14] In a study from Germany, Sommer et al. noted that hospitalized treatment-resistant patients with chronic plaque psoriasis were significantly more likely (odds ratio: 5.92) to have metabolic syndrome as compared to controls and this correlation was stronger for patients with greater body surface area involvement.[15] They did not observe any difference in the prevalence of metabolic syndrome amongst patients who had had their psoriasis for less than or more than 15 years. However, 15 years may have been too long a cut-off period as it probably takes the inflammatory triggers of psoriasis much less time to initiate metabolic syndrome. Langan et al. also observed an increasing trend of the presence of metabolic syndrome with increasing severity of psoriasis.[16] However, in this study based on retrieval of computerized medical records, only psoriasis patients aged 45–65 years were included.
There is a paucity of studies from India on the prevalence of metabolic syndrome in psoriasis patients. Nisa and Qazi reported an increased prevalence of metabolic syndrome in patients with psoriasis (28%) as compared to controls (6%) with an odds ratio of 6.09.[7] The high odds ratio in their study may be attributable to the high psoriasis area and severity index (PASI) scores (mean, 15.2 ± 13.9 and median, 13.05) of their patients, comparable to the scores of the patients with severe psoriasis in the present study (odds ratio of 7.2 for developing metabolic syndrome). However, Pereira et al. in a study on 77 patients with chronic plaque psoriasis from Mumbai, India and Lakshmi et al. in a study of 40 patients with chronic plaque psoriasis from South India were not able to demonstrate any significant association between metabolic syndrome and psoriasis in comparison to controls.[8],[12] More recently, Madanagobalane and Anandan with the use of the South Asian-modified National Cholesterol Education Program's Adult Treatment Panel III criteria observed that metabolic syndrome was significantly more common in psoriasis patients (44.1%) than in controls (30%) but did not note any correlation with severity.[9] Sharma et al. had also shown increased risk of metabolic syndrome in patients with psoriasis, especially in those with long-standing psoriasis and active joint disease.[11]
There is substantial data to suggest that prevalence of various components of metabolic syndrome is higher in patients with psoriasis. From India, while Madanagobalane and Anandan, reported a higher prevalence of obesity in psoriasis patients than in controls, Nisa and Qazi did not observe any such difference in the occurrence of central obesity.[7],[9] The latter study needs to be interpreted keeping in mind the National Family Health Survey 2007 report in which a relatively lower prevalence of obesity was reported in the general population in Jammu and Kashmir (8.7%) compared to other North Indian states. We observed a linear relationship between the severity of psoriasis and prevalence of hypertension and diabetes. Though several studies from the West have shown an association between hypertension and psoriasis, Indian studies have been equivocal.[15],[17],[18] However, the studies by Pereira et al., Madanagobalane and Anandan, Nigam and Dayal and Sundharam et al. corroborate our observations on the association of psoriasis and diabetes.[8],[9],[19],[20] Langan et al. noted a similar relationship of severity of psoriasis to the presence of obesity, hypertension and elevated fasting blood sugar.[16] However, they categorized the severity of disease based on the percentage of body surface area involvement which may be a poor marker of the severity of inflammation. Of all the components of metabolic syndrome, inconsistencies across various studies are maximal with respect to dyslipidemia, with some studies indicating an association of dyslipidemia with psoriasis and others noting an association with respect to levels of some components of serum lipids.[7],[9],[15],[16],[18],[21] However, several workers were not able to corroborate these findings.[8],[22],[23],[24]
In keeping with our findings, a study from Israel also observed higher electrocardiographic abnormalities in patients with psoriatic arthritis when compared to controls.[25] Nearly more than a fifth had abnormal echocardiogram findings in comparison to 6.7% of controls (P = 0.07). Similar findings have been reported by Biyik et al. in a study of 216 Turkish patients with psoriasis.[26] These are the only available reports on electrocardiographic and echocardiographic abnormalities in psoriasis patients. In these societies, smoking is known to be nonexistent/very low, whereas our patient series showed a 37% prevalence of smoking. Our results indicate that smoking could be an additional contributor for electrocardiographic and echocardiogram abnormalities in chronic plaque psoriasis. However, this needs to be confirmed in other Indian settings with large sample sizes and long follow-up.
Our findings are also consistent with previous studies of Gonzalez–Juanatey et al., Yiu et al. and Mongy et al. all of whom had also observed carotid plaques in their patients with psoriasis.[6],[27],[28] Karoli et al. in a study of 100 patients from India had shown that in patients with psoriasis, carotid intima-media thickness was associated with increased severity and duration of psoriasis.[10] There was no significant correlation in electrocardiography, echocardiogram and carotid intima-media thickness findings in the present as well as previous studies.[6],[28]
A limitation of our study, since it was cross-sectional, was that it does not take into account the directionality of the association to be set. The hypothesis that metabolic syndrome can occur more frequently in psoriasis needs to be validated in large prospective studies.
Conclusion
We found a higher prevalence of metabolic syndrome and its individual components in patients with psoriasis; these could play a role in accelerating the development of atherosclerosis. Though the association was seen at all severities of psoriasis, it increased as severity increased.
We also observed a significant increase in carotid artery intima-media thickness in psoriasis patients. There is a paucity of data on cardiovascular changes and prevalence of subclinical atherosclerosis in patients with psoriasis in comparison to controls in the Indian population but our study suggests a need to evaluate these aspects further with larger, prospective studies.
We suggest that patients with moderate to severe psoriasis and those with psoriasis for longer than 3 years be screened routinely for metabolic syndrome and cardiovascular disease and also be encouraged to correct their modifiable cardiovascular risk factors aggressively.
Acknowledgment
We would like to thank the Indian Council of Medical Research for providing a grant to conduct this study.
Financial support and sponsorship
The Indian Council of Medical Research awarded an MD Thesis Grant of 25,000 INR for this study. It was given in two phases – first (15,000 INR) during the study and second (10,000 INR) after completion of the study.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Neimann AL, Porter SB, Gelfand JM. Epidemiology of psoriasis. Expert Rev Dermatol 2006;1:63-75.
[Google Scholar]
|
| 2. |
Rapp SR, Feldman SR, Exum ML, Fleischer AB Jr, Reboussin DM. Psoriasis causes as much disability as other major medical diseases. J Am Acad Dermatol 1999;41 (3 Pt 1):401-7.
[Google Scholar]
|
| 3. |
Neimann AL, Shin DB, Wang X, Margolis DJ, Troxel AB, Gelfand JM. Prevalence of cardiovascular risk factors in patients with psoriasis. J Am Acad Dermatol 2006;55:829-35.
[Google Scholar]
|
| 4. |
Mallbris L, Ritchlin CT, Ståhle M. Metabolic disorders in patients with psoriasis and psoriatic arthritis. Curr Rheumatol Rep 2006;8:355-63.
[Google Scholar]
|
| 5. |
Cohen AD, Sherf M, Vidavsky L, Vardy DA, Shapiro J, Meyerovitch J. Association between psoriasis and the metabolic syndrome. A cross-sectional study. Dermatology 2008;216:152-5.
[Google Scholar]
|
| 6. |
Gonzalez-Juanatey C, Llorca J, Amigo-Diaz E, Dierssen T, Martin J, Gonzalez-Gay MA. High prevalence of subclinical atherosclerosis in psoriatic arthritis patients without clinically evident cardiovascular disease or classic atherosclerosis risk factors. Arthritis Rheum 2007;57:1074-80.
[Google Scholar]
|
| 7. |
Nisa N, Qazi MA. Prevalence of metabolic syndrome in patients with psoriasis. Indian J Dermatol Venereol Leprol 2010;76:662-5.
[Google Scholar]
|
| 8. |
Pereira RR, Amladi ST, Varthakavi PK. A study of the prevalence of diabetes, insulin resistance, lipid abnormalities, and cardiovascular risk factors in patients with chronic plaque psoriasis. Indian J Dermatol 2011;56:520-6.
[Google Scholar]
|
| 9. |
Madanagobalane S, Anandan S. Prevalence of metabolic syndrome in South Indian patients with psoriasis vulgaris and the relation between disease severity and metabolic syndrome: A hospital-based case-control study. Indian J Dermatol 2012;57:353-7.
[Google Scholar]
|
| 10. |
Karoli R, Fatima J, Shukla V, Dhillon KS, Khanduri S, Maini S, et al. Astudy of cardio-metabolic risk profile in patients with psoriasis. J Assoc Physicians India 2013;61:798-803.
[Google Scholar]
|
| 11. |
Sharma A, Gopalakrishnan D, Kumar R, Vijayvergiya R, Dogra S. Metabolic syndrome in psoriatic arthritis patients: A cross-sectional study. Int J Rheum Dis 2013;16:667-73.
[Google Scholar]
|
| 12. |
Lakshmi S, Nath AK, Udayashankar C. Metabolic syndrome in patients with psoriasis: A comparative study. Indian Dermatol Online J 2014;5:132-7.
[Google Scholar]
|
| 13. |
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005;112:2735-52.
[Google Scholar]
|
| 14. |
Gisondi P, Tessari G, Conti A, Piaserico S, Schianchi S, Peserico A, et al. Prevalence of metabolic syndrome in patients with psoriasis: A hospital-based case-control study. Br J Dermatol 2007;157:68-73.
[Google Scholar]
|
| 15. |
Sommer DM, Jenisch S, Suchan M, Christophers E, Weichenthal M. Increased prevalence of the metabolic syndrome in patients with moderate to severe psoriasis. Arch Dermatol Res 2006;298:321-8.
[Google Scholar]
|
| 16. |
Langan SM, Seminara NM, Shin DB, Troxel AB, Kimmel SE, Mehta NN, et al. Prevalence of metabolic syndrome in patients with psoriasis: A population-based study in the United Kingdom. J Invest Dermatol 2012;132(3 Pt 1):556-62.
[Google Scholar]
|
| 17. |
Love TJ, Qureshi AA, Karlson EW, Gelfand JM, Choi HK. Prevalence of the metabolic syndrome in psoriasis: Results from the national health and nutrition examination survey, 2003-2006. Arch Dermatol 2011;147:419-24.
[Google Scholar]
|
| 18. |
Shapiro J, Cohen AD, Weitzman D, Tal R, David M. Psoriasis and cardiovascular risk factors: A case-control study on inpatients comparing psoriasis to dermatitis. J Am Acad Dermatol 2012;66:252-8.
[Google Scholar]
|
| 19. |
Nigam P, Dayal SG. Diabetic status in psoriasis. Indian J Dermatol Venereol Leprol 1979;45:171-4.
[Google Scholar]
|
| 20. |
Sundharam A, Singh R, Agarwal PS. Psoriasis and diabetes mellitus. Indian J Dermatol Venereol Leprol 1980;46:158-62.
[Google Scholar]
|
| 21. |
Mallbris L, Granath F, Hamsten A, Ståhle M. Psoriasis is associated with lipid abnormalities at the onset of skin disease. J Am Acad Dermatol 2006;54:614-21.
[Google Scholar]
|
| 22. |
Farshchian M, Zamanian A, Farshchian M, Monsef AR, Mahjub H. Serum lipid level in Iranian patients with psoriasis. J Eur Acad Dermatol Venereol 2007;21:802-5.
[Google Scholar]
|
| 23. |
Seçkin D, Tokgözoglu L, Akkaya S. Are lipoprotein profile and lipoprotein (a) levels altered in men with psoriasis? J Am Acad Dermatol 1994;31 (3 Pt 1):445-9.
[Google Scholar]
|
| 24. |
Bedi TR. Blood sugar and serum cholesterol levels in psoriasis. Indian J Dermatol Venereol Leprol 1979;45:272-3.
[Google Scholar]
|
| 25. |
Feld J, Weiss G, Rosner I, Rozenbaum M, Laor A, Rimar D, et al. Electrocardiographic findings in psoriatic arthritis: A case-controlled study. J Rheumatol 2008;35:2379-82.
[Google Scholar]
|
| 26. |
Biyik I, Narin A, Bozok MA, Ergene O. Echocardiographic and clinical abnormalities in patients with psoriasis. J Int Med Res 2006;34:632-9.
[Google Scholar]
|
| 27. |
Yiu KH, Yeung CK, Zhao CT, Chan JC, Siu CW, Tam S, et al. Prevalence and extent of subclinical atherosclerosis in patients with psoriasis. J Intern Med 2013;273:273-82.
[Google Scholar]
|
| 28. |
El-Mongy S, Fathy H, Abdelaziz A, Omran E, George S, Neseem N, et al. Subclinical atherosclerosis in patients with chronic psoriasis: A potential association. J Eur Acad Dermatol Venereol 2010;24:661-6.
[Google Scholar]
|
Fulltext Views
3,220
PDF downloads
977





