Translate this page into:
Idiopathic eruptive macular pigmentation: A critical review of published literature and suggestions for revision of criteria for diagnosis
2 Department of Dermatology Venereology and Leprosy, MGM Medical College, Navi Mumbai, Maharashtra, India
Correspondence Address:
Rajiv Sharad Joshi
14, Jay Mahal, A Road, Churchgate, Mumbai - 400 020, Maharashtra
India
| How to cite this article: Joshi RS, Rohatgi S. Idiopathic eruptive macular pigmentation: A critical review of published literature and suggestions for revision of criteria for diagnosis. Indian J Dermatol Venereol Leprol 2015;81:576-580 |
Idiopathic eruptive macular pigmentation is an uncommon, probably under-reported condition that has been described mostly in children and adolescents who present with multiple discrete asymptomatic brown-black macules and flat plaques on the face, trunk and proximal extremities without any preceding inflammation or drug exposure. The eruption persists for variable periods of time and, in most cases, has been recorded to clear spontaneously without any residual changes of pigmentation or scarring.
The term idiopathic eruptive macular pigmentation was first proposed by Degos et al. in 1978, and several cases were described in the French literature.[1] The first English language report of 5 cases was by Sanz de Galdeano et al. in 1996, who proposed diagnostic criteria for this entity which have been widely quoted in subsequent literature on the subject.[2]
Clinically, the skin lesions closely resemble and are, therefore, often wrongly diagnosed as lichen planus pigmentosus, ashy dermatosis, fixed drug eruptions, urticaria pigmentosa and post-inflammatory pigmentation. Histology is necessary to differentiate idiopathic eruptive macular pigmentation from the diseases mentioned above. Most authors have described epidermal hypermelanosis as the most prominent finding in idiopathic eruptive macular pigmentation.
Epidermal hypermelanosis with papillomatosis (pigmented papillomatosis) as the characteristic histological finding in idiopathic eruptive macular pigmentation was described in 2007. Since then, several cases of idiopathic eruptive macular pigmentation have been described with pigmented papillomatosis.[3],[4],[5],[6],[7]
A perusal of literature on the subject suggests that several of the cases described as idiopathic eruptive macular pigmentation actually show features of dermal melanosis and are not idiopathic eruptive macular pigmentation but likely to be ashy dermatosis, lichen planus pigmentosus and post-inflammatory pigmentation.
In this article, we critically examine the criteria that are used to diagnosis idiopathic eruptive macular pigmentation and suggest a revision of criteria to diagnose with specificity the entity of idiopathic eruptive macular pigmentation.
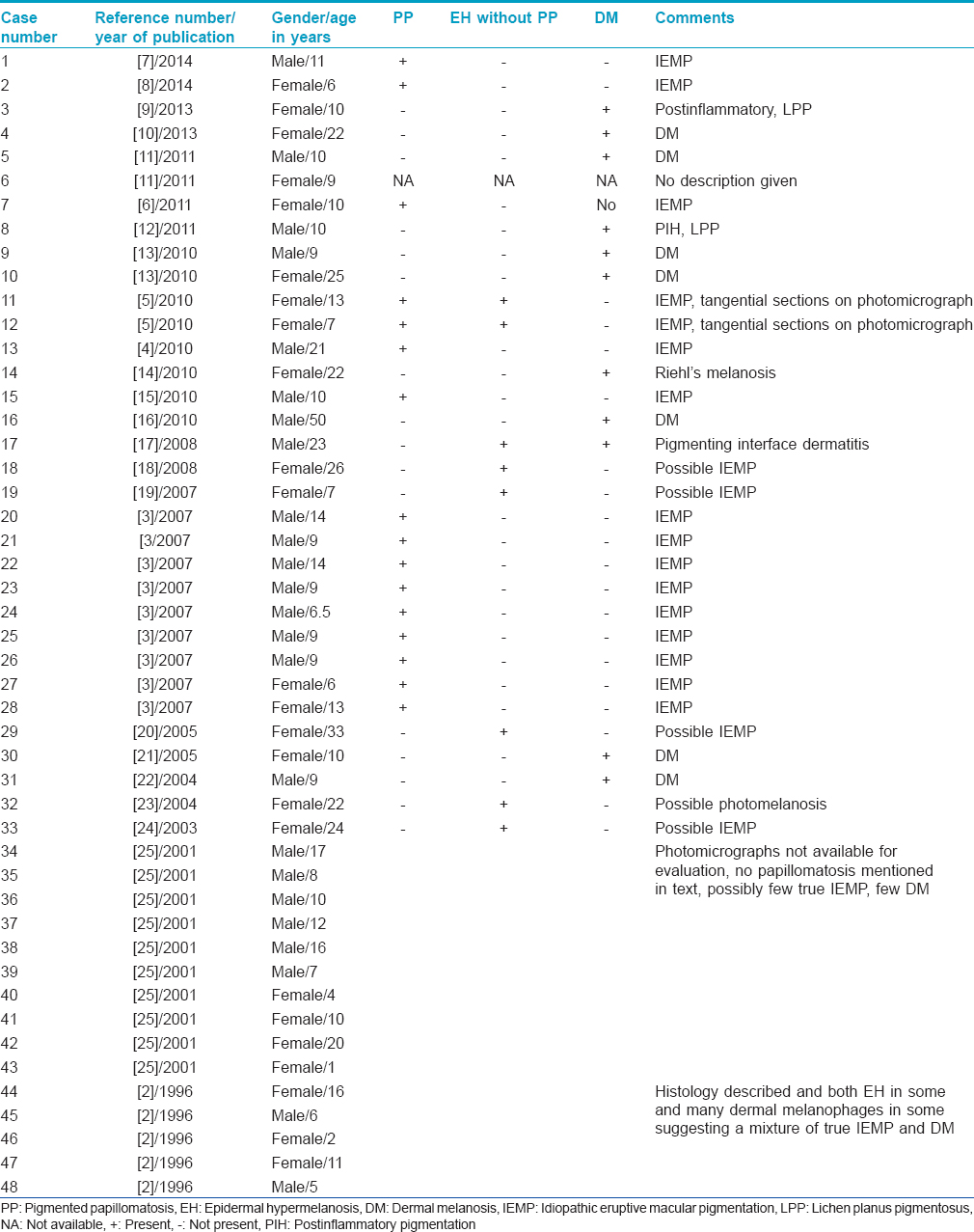
PubMed search for the key words idiopathic eruptive macular pigmentation yielded 24 articles in English with 48 cases of idiopathic eruptive macular pigmentation.
A review of the case reports with particular attention to the histological features described and study of clinical photographs and photomicrographs, where available, was done. The cases were classified as (a) idiopathic eruptive macular pigmentation with pigmented papillomatosis, (b) possible idiopathic eruptive macular pigmentation with epidermal pigmentation but no mention of papillomatosis and (c) dermal melanoses with prominent incontinence of melanin in the papillary dermis with or without interface changes.
Twenty-four articles were retrieved and these described 48 cases of idiopathic eruptive macular pigmentation [Table - 1]. Sixteen cases were deemed to be idiopathic eruptive macular pigmentation with pigmented papillomatosis as the main diagnostic feature on histopathology. Twenty cases were considered to be possible idiopathic eruptive macular pigmentation as they had increased epidermal melanin. However, there was no mention of papillomatosis of the epidermis. Twelve cases showed features of dermal melanosis with many melanophages in the papillary dermis and were classified as dermal melanosis and were considered to be entities other than idiopathic eruptive macular pigmentation. In the idiopathic eruptive macular pigmentation with papillomatosis group, 10 were males and 6 were females. The age distribution was 10 cases below the age of 10 years, 5 cases between 11 years and 14 years and a solitary young man of 21 years. Nineteen cases were published after 2007 (after description of pigmented papillomatosis as the histological finding in idiopathic eruptive macular pigmentation). Of them, one had no histological description except the statement that the findings were consistent with idiopathic eruptive macular pigmentation. Of the remaining 18 which could be evaluated by description/photomicrographs, 9 (50%) cases were deemed to be dermal melanosis and not true idiopathic eruptive macular pigmentation.
Sanz de Galdeano et al. in 1996 suggested the following criteria for diagnosis of idiopathic eruptive macular pigmentation.[2] (1) Eruption of brownish-black discrete, non-confluent asymptomatic macules involving the neck, trunk and proximal extremities in children and adolescents. (2) Absence of any preceding inflammatory lesions. (3) No previous drug exposure. (4) Basal cell hyperpigmentation of the epidermis with dermal melanophages without any basal cell damage or lichenoid infiltrate. (5) Normal mast cell counts. These criteria were based on history, clinical presentation and histological findings in the 5 cases that they published. Subsequently, all publications on the subject have quoted these criteria for diagnosis of idiopathic eruptive macular pigmentation.
We will discuss these criteria individually and suggest changes and additions to them to enable specific diagnosis of idiopathic eruptive macular pigmentation, because at least 12 of 48 cases (25%) in our opinion were wrongly diagnosed as idiopathic eruptive macular pigmentation. If cases described after 2007 are considered, as many as 50% (9 of 18) cases are dermal melanosis and not idiopathic eruptive macular pigmentation.
The first criterion describing the clinical presentation of patients with idiopathic eruptive macular pigmentation may be modified to also include the presence of slightly raised plaques that resemble acanthosis nigricans as this finding has been reported in several cases of idiopathic eruptive macular pigmentation reported after 2007. This criterion, therefore, may read as“eruption of brownish-black discrete, non-confluent asymptomatic macules and slightly raised plaques that resemble acanthosis nigricans and involve the face, neck, trunk and proximal extremities.”
Criteria 2, 3 and 5 may be retained as they historically rule out preceding inflammation or drug reactions as cause of the hyperpigmentation and normal mast cell counts in the dermis rules out urticaria pigmentosa.
Idiopathic eruptive macular pigmentation as we understand it is an epidermal hypermelanotic condition. Several cases with papillomatosis (pigmented papillomatosis) have been described, a finding that is, similar to acanthosis nigricans, confluent and reticulate papillomatosis and some epidermal nevi. There is no dermal inflammation, no interface dermatitis and no melanophages in the papillary dermis. Melanophages, if present, are a few and may reflect localized inflammation and may be considered as incidental.
Findings of numerous melanophages in the papillary dermis or a significant inflammatory infiltrate or interface changes suggests a dermal melanotic condition such as lichen planus pigmentosus, ashy dermatosis and Riehl's melanosis and should be considered as a negative criterion and against the diagnosis of idiopathic eruptive macular pigmentation.
Furthermore, because histology is essential to differentiate idiopathic eruptive macular pigmentation from the more common dermal melanotic conditions, epidermal hypermelanosis with or without pigmented papillomatosis in the absence of significant dermal inflammatory infiltrate, interface changes and dermal melanophages should be the primary criterion for diagnosis.
As this condition has been described mainly in children and adolescents and most cases reported in adults seem to be dermal melanosis and not idiopathic eruptive macular pigmentation, inclusion of age as a defining criterion seems warranted.[13],[14],[16],[17],[23]
It is possible that two different entities have been described under the term idiopathic eruptive macular pigmentation. One that has epidermal hypermelanosis without papillomatosis (macular idiopathic eruptive macular pigmentation) and the other with epidermal papillomatosis resembling acanthosis nigricans (pigmented papillomatosis). Both entities, however, are epidermal hypermelanotic conditions occurring mainly in children and adolescents. Moreover as more cases are described, it may be possible to either differentiate them as separate entities or merge them into the same rubric, idiopathic eruptive macular pigmentation.
In sum, therefore, we suggest that the following modification of criteria for diagnosis of idiopathic eruptive macular pigmentation be used for specific diagnosis of this uncommon and probably under-reported entity in young children and adolescents.
- Eruption of brownish-black discrete, non-confluent asymptomatic macules and/or slightly raised plaques that resemble acanthosis nigricans and involve the face, neck, trunk and proximal extremities, with complete resolution after months or years
- Affecting mostly children and adolescents, that is, the first two decades of life
- Epidermal hypermelanosis with or without papillomatosis as the main histological finding with absence of dermal inflammation
- Numerous dermal melanophages and the presence of interface changes are negative findings and may be considered to be against the diagnosis of idiopathic eruptive macular pigmentation
- Absence of preceding inflammatory lesions
- No previous drug exposure
- Normal mast cell counts.
Conclusions and Comments
A major limitation of this study is that clinical photographs and photomicrographs are not available for many cases and the description of the histology is sketchy and difficult to evaluate in some cases.
Our review suggests that almost 25% of cases published as idiopathic eruptive macular pigmentation are actually dermal melanoses, (50% if cases published after 2007 are considered) and have been included as idiopathic eruptive macular pigmentation due to ambiguous criterion of dermal melanophages in the original description by Sanz de Galdeano. Several of the cases described in literature as idiopathic eruptive macular pigmentation show features of dermal melanosis as is evident from the published photomicrographs. Many cases do not have photomicrographs and could not be evaluated except based on the description in the text. Moreover, it is possible that some of the cas es of possible idiopathic eruptive macular pigmentation may have been dermal melanotic conditions.
Histopathology is the most important investigation for differentiating idiopathic eruptive macular pigmentation from the other clinical differential diagnoses. Idiopathic eruptive macular pigmentation is an epidermal hypermelanosis and this should be the primary criterion for the diagnosis. The presence of pigmented papillomatosis may reflect an entity different from macular idiopathic eruptive macular pigmentation. However, since the description of pigmented papillomatosis in 2007, most cases of idiopathic eruptive macular pigmentation (7 of 9) have been described with this histological finding.
On the other hand, prominent dermal inflammatory infiltrate, many melanophages or interface changes are findings against the diagnosis of idiopathic eruptive macular pigmentation. Confluent pigmentation is unlikely to be idiopathic eruptive macular pigmentation and if accompanied by histological findings of dermal melanosis is almost definitely lichen planus pigmentosus or Riehl's melanosis.
We suggest, therefore, modification of the diagnostic criteria for the diagnosis of idiopathic eruptive macular pigmentation with emphasis on the histological findings of pigmented papillomatosis and hope that adoption of these will help in specific diagnosis of this condition.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.[25]
| 1. |
Degos R, Civatte J, Belaïch S. Idiopathic eruptive macular pigmentation (author's transl). Ann Dermatol Venereol 1978;105:177-82.
[Google Scholar]
|
| 2. |
Sanz de Galdeano C, Léauté-Labrèze C, Bioulac-Sage P, Nikolic M, Taïeb A. Idiopathic eruptive macular pigmentation: Report of five patients. Pediatr Dermatol 1996;13:274-7.
[Google Scholar]
|
| 3. |
Joshi R. Idiopathic eruptive macular pigmentation with papillomatosis: Report of nine cases. Indian J Dermatol Venereol Leprol 2007;73:402-5.
[Google Scholar]
|
| 4. |
Joshi R, Palwade PK. Idiopathic eruptive macular pigmentation or acanthosis nigricans? Indian J Dermatol Venereol Leprol 2010;76:591.
[Google Scholar]
|
| 5. |
Grover S, Basu A. Idiopathic eruptive macular pigmentation: Report on two cases. Indian J Dermatol 2010;55:277-8.
[Google Scholar]
|
| 6. |
Verma S, Thakur BK. Idiopathic eruptive macular pigmentation with papillomatosis. Indian Dermatol Online J 2011;2:101-3.
[Google Scholar]
|
| 7. |
Begum A, Ramchandra BV, Kumar A. Idiopathic eruptive macular pigmentation. Indian J Paediatr Dermatol 2014;15:114-6.
[Google Scholar]
|
| 8. |
Herd TJ, Wright TS. Idiopathic eruptive macular pigmentation involving the distal extremities: A case report. Pediatr Dermatol 2014;31:e52-4.
[Google Scholar]
|
| 9. |
Kim S, Sun G, Brandon K. Idiopathic eruptive macular pigmentation. J Am Acad Dermatol 2013;68(Suppl 1):AB174.
[Google Scholar]
|
| 10. |
Oiso N, Kawada A. Idiopathic eruptive macular pigmentation following a Christmas tree pattern. J Dermatol 2013;40:934-5.
[Google Scholar]
|
| 11. |
Rodriguez VG, Gonzalez JE, Wong CL, Gonzalez FK, Candiani JO, Flores MG. Idiopathic eruptive macular pigmentation: A diagnostic challenge. J Am Acad Dermatol 2011;64:AB132.
[Google Scholar]
|
| 12. |
Komorowska O, Szczerlowska-Dobosz A, Roziewska D, Czapiewski P. Idiopathic eruptive macular pigmentation: A rare pigmentary disorder. Adv Dermatol Allergol 2011;2:150-3.
[Google Scholar]
|
| 13. |
Kim KF, Cho BK, Park HJ. Idiopathic eruptive macular pigmentation: Report of two cases. J Am Acad Dermatol 2010;62:AB120.
[Google Scholar]
|
| 14. |
de Souza DF, Cunha AC, Piñeiro-Maceira J, Gomes MK, Sodré CT, Ramos-e-Silva M. Idiopathic eruptive macular pigmentation associated with pregnancy. Int J Dermatol 2010;49:810-2.
[Google Scholar]
|
| 15. |
Chiu MW, Suh KY, Pirouzmanesh A, Landau JW. Multiple brown patches on the trunk. Idiopathic eruptive macular pigmentation with papillomatosis (IEMP). Arch Dermatol 2010;146:1301-6.
[Google Scholar]
|
| 16. |
Mantovani L, Minghetti S, Ricci M, Zauli S, Marzola A, Corazza M. Idiopathic eruptive macular pigmentation in a 50-year-old man. Eur J Dermatol 2010;20:633-4.
[Google Scholar]
|
| 17. |
Câmara VM, Lupi O, Piñeiro-Maceira J. Idiopathic eruptive macular pigmentation. Int J Dermatol 2008;47:272-5.
[Google Scholar]
|
| 18. |
Kim EH, Lee ES, Kim YC, Kang HY. A case of idiopathic eruptive macular pigmentation limited to flexural areas. Ann Dermatol (Seoul) 2008;20:98-101.
[Google Scholar]
|
| 19. |
Volz A, Metze D, Böhm M, Bruckner-Tuderman L, Nashan D. Idiopathic eruptive macular pigmentation in a 7-year-old girl: Case report and discussion of differences from erythema dyschromicum perstans. Br J Dermatol 2007;157:839-40.
[Google Scholar]
|
| 20. |
Milobratovic D, Djordjevic S, Vukicevic J, Bogdanovic Z. Idiopathic eruptive macular pigmentation associated with pregnancy and Hashimoto thyroiditis. J Am Acad Dermatol 2005;52:919-21.
[Google Scholar]
|
| 21. |
Trcko K, Marko PB, Miljkovic J. Idiopathic eruptive macular pigmentation. Acta Dermatovenerol Alp Pannonica Adriat 2005;14:30-4.
[Google Scholar]
|
| 22. |
Guil FM, Falcon CS, Sanchez GS, Campos CD, Solano JL, Sintes RN. Idiopathic eruptive macular pigmentation. Med Cutan Ibero Lat Am 2004;32:124-7.
[Google Scholar]
|
| 23. |
Yoon TY, Lee GC, Kim YG, Kim MK, Kim CY. A case of idiopathic eruptive macular pigmentation. J Dermatol 2004;31:440-1.
[Google Scholar]
|
| 24. |
Mehta S, Aasi S, Cole R, Chu P, Weinberg JM. Idiopathic eruptive macular pigmentation: A case of 21 years' duration. J Am Acad Dermatol 2003;49 5 Suppl: S280-2.
[Google Scholar]
|
| 25. |
Jang KA, Choi JH, Sung KS, Moon KC, Koh JK. Idiopathic eruptive macular pigmentation: Report of 10 cases. J Am Acad Dermatol 2001;44 2 Suppl: 351-3.
[Google Scholar]
|
Fulltext Views
3,917
PDF downloads
1,301





