Translate this page into:
Clinical and histological patterns of dermatofibroma without gross skin surface change: A comparative study with conventional dermatofibroma
Correspondence Address:
Mi Woo Lee
Department of Dermatology, Asan Medical Center, University of Ulsan College of Medicine, 388-1 Pungnapdong Songpagu, Seoul, 138-736
Korea
| How to cite this article: Lee WJ, Jung JM, Won CH, Chang SE, Choi JH, Moon KC, Lee MW. Clinical and histological patterns of dermatofibroma without gross skin surface change: A comparative study with conventional dermatofibroma. Indian J Dermatol Venereol Leprol 2015;81:263-269 |
Abstract
Background : Dermatofibroma sometimes clinically presents as a nodular lesion without gross skin surface change. Clinicopathologic features of this variant of dermatofibroma have not been evaluated. Aims : To assess clinicopathologic features of dermatofibroma presenting as a subcutaneous nodule. Methods : This study reviewed the clinical and histological features of 42 cases of subcutaneous dermatofibromas and compared them with 95 cases of conventional dermatofibroma. Results : Dermatofibroma without gross skin surface change was associated with a shorter pre-diagnosis duration than conventional dermatofibroma. Increase in size during the pre-diagnosis period was significantly more frequent in the conventional type. In addition, these dermatofibromas were more likely than the conventional type to occur in the head and neck region. Although tumor depth was deeper than in the conventional type, less than half of the dermatofibromas without gross skin surface change were found histologically to be "subcutaneous" or "deep-penetrating dermatofibroma". Subcutaneous extension was more frequent in these dermatofibromas while focal stromal hyalinization and hemosiderin deposits were more common in the conventional type. Limitations: This study is a retrospective, single center design. Conclusion : The present study suggests that dermatofibroma without gross skin surface change is a variant type with distinct clinical and histological features that distinguish them from conventional dermatofibroma.INTRODUCTION
Dermatofibromas (benign fibrous histiocytoma) are usually confined to the dermis, and most cases are not difficult to diagnose clinically. Dermatofibroma is commonly associated with epidermal-hyperplasia and basal pigmentation. This is reflected clinically by the brownish discoloration and/or scaling seen on the surface of the elevated or atrophic skin lesions. [1] Although there is little difficulty in diagnosing dermatofibroma when it presents with typical skin surface changes, nodular lesions without gross skin surface change can be problematic. Dermatofibroma without gross skin surface change appears uncommon and this might explain the lack of published analyses of the clinicohistologic features of this variant. Histological variants with deep subcutaneous extension, so called "deep-penetrating dermatofibroma", and "purely subcutaneous dermatofibroma" have been described. [2],[3],[4],[5],[6] However, only two series comprising of 21 and 69 cases arising in subcutaneous tissue and deep soft tissue have been published. [2],[3] "Subcutaneous" and "deep-penetrating dermatofibroma" are known to have a higher risk of local recurrence than conventional cutaneous dermatofibroma. [3],[7] However, clinical features of dermatofibromas histologically located entirely within subcutaneous tissue have not been evaluated.
Since the histologic features of dermatofibroma without gross skin surface change have not been analyzed, it is unclear whether they differ from the conventional type. We compared the clinical and histologic features of both these types of dermatofibromas.
METHODS
We performed a retrospective evaluation of 672 dermatofibroma cases diagnosed at Asan Medical Center in Korea between June 2003 and July 2013. The pathological diagnosis of dermatofibroma was based on histopatholoical evaluation of the typical features along with detection of the typical immunophenotypical characteristics: factor XIIIa positivity and CD34 negativity. Cases of nodular fasciitis, dermatofibrosarcoma protuberans and malignant fibrous histiocytoma were excluded from our study. Dermatofibromas clinically presenting as a nodular lesion without gross skin surface changes such as depression, elevation, and pigmentation were included in the study. Ninety-five cases of conventional dermatofibroma were randomly selected from the diagnosed population and included to allow for a comparison of clinico-histopathologic features.
We collected and compared clinical data (age, sex, distribution of lesions, size of lesions, lesion-related symptoms, pre-diagnosis duration, increase in lesion size during the disease course, and follow-up information) and histologic features (depth of tumor, extension into the subcutaneous layer, cellular polymorphism, and mitoses, and histologic variants, such as cellular, aneurysmal, and atypical dermatofibroma). Cases were excluded from study if medical records did not detail these clinical and histologic features. Tumor depth was assessed by measuring the distance from the top of the granular layer to the upper margin of the tumor using a scale mounted in the eyepiece of the microscope. All specimens were fixed in formalin, embedded in paraffin, and stained for hematoxylin and eosin. This study was approved by the Institutional Review Board of our institution and was performed in accordance with the ethical standards of the Helsinki Declaration of 1975 .
Statistical analysis
All data were statistically analyzed using SPSS version 18.0 (SPSS Inc., Chicago, IL). A P < 0.05 were considered to indicate statistical significance. Differences in age of patients, pre-diagnosis duration and tumor depth between dermatofibroma without gross skin surface change and conventional type were examined using the Student t-test. Other clinical and histologic features were analyzed using Chi-square test, Fisher′s exact test, or linear by linear association test.
RESULTS
Frequency and clinical features
Of 672 diagnosed cases, 42 (6.3%) were dermatofibromas without gross skin surface change [Figure - 1]. The clinical features of patients in this study are summarized in [Table - 1]. The mean age at presentation was 40.6 years (range, 6-67 years) in those with dermatofibroma without gross skin surface change and 41.1 years (range, 11-72 years) in those with the conventional type. This difference was not significant (P = 0.848). There were more females than males in both groups; 29 (69%) of 42 patients with dermatofibroma without gross skin surface change and 68 (72%) of 95 patients with the conventional type. The clinical diagnosis of dermatofibroma was made in 5 (12%) of 42 patients and in 83 (87%) of 95 patients with dermatofibroma without gross skin surface change and conventional dermatofibroma, respectively. Lipoma (n = 14), epidermal cyst (n = 13), leiomyoma (n = 3) and panniculitis (n = 2) were clinically suspected in the former group and no clinical diagnosis was given in five of these cases.
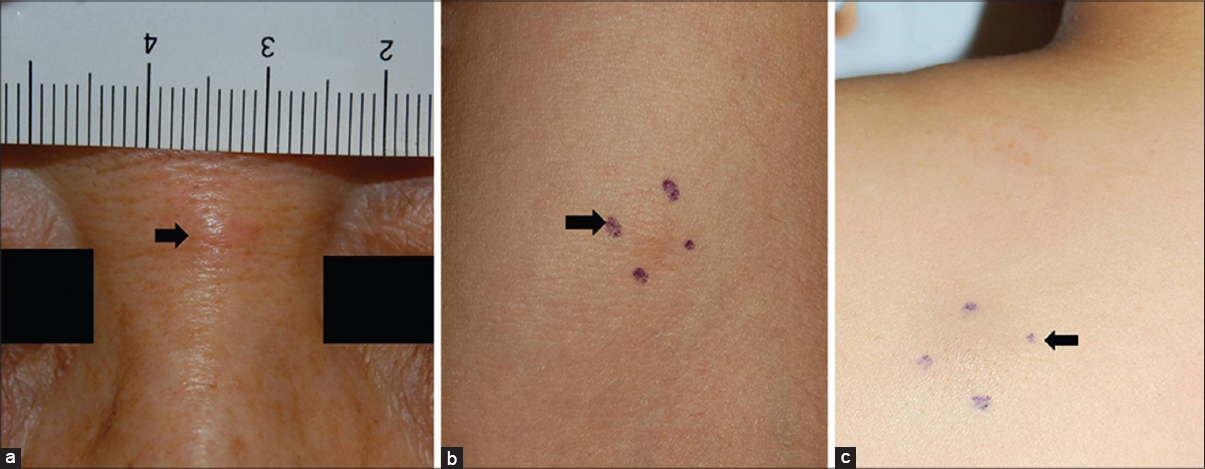 |
| Figure 1: Clinical manifestations of dermatofibroma without gross skin surface change. A subcutaneous nodule on (a) the nasal root, (b) right forearm, and (c) upper back |

Anatomic distribution
There was a significant difference in the anatomic distribution of dermatofibroma without gross skin surface change and conventional type (P < 0.001). The former were commonly found in the head and neck region (18 of 42, 43%), but the conventional type were more frequent in the lower extremities (51 of 95, 54%).
Lesion-related symptoms
The frequency of related symptoms in patients with dermatofibroma without gross skin surface change and in those with conventional type were similar (P = 0.315). Five (12%) patients in the former group experienced pain or tenderness and five (12%) experienced pruritus. Pain or tenderness was noted in 21 (22%) patients who had conventional dermatofibroma and pruritus was noted in 10 (11%).
Pre-diagnosis duration
The duration of lesions prior to visiting the clinic ranged from 1 month to 2 years (median, 5.84 months) for dermatofibroma without gross skin surface change and from 1 month to 10 years (median, 26.41 months) for the conventional type. Pre-diagnosis duration was significantly longer in the conventional type (P < 0.001).
Size change during the disease course
The size of lesions was available in 33 and 82 patients with dermatofibroma without gross skin surface change and conventional dermatofibroma, respectively. The size was significantly larger for the conventional type (mean size, 1.21 ± 0.41 cm) than for the former group (mean size, 0.79 ± 0.19 cm) (P = 0.038). The size of lesions increased in 11 (26%) of 42 patients who had dermatofibroma without gross skin surface change and in 53 (56%) of 95 patients with the conventional type. This difference was statistically significant (P = 0.003).
Follow-up data
The dermatofibromas were subsequently excised after the initial biopsy in 62 cases (13 cases of dermatofibroma without gross skin surface change and 49 cases of conventional dermatofibroma). Given the benign nature of this tumor, many patients did not attend follow-up examinations. Because of that, follow-up information was available for only 9 cases of dermatofibroma without gross skin surface change and 29 cases of conventional type. Local recurrence and distant metastases did not occur in any of the patients.
Histologic features
The histologic features analyzed in the present study are summarized in [Table - 1]. All dermatofibromas were characterized as a poorly circumscribed proliferation of spindle-shaped fibroblasts or histiocytes arranged in sheets or interlocking strands with a storiform pattern, entrapment of collagen bundles, and patchy lymphocyte infiltrates. Cytologically, the tumors were dominated by plump, ovoid to spindle-shaped cells with pale, eosinophilic cytoplasm and bland nuclei with vesicular chromatin.
Epidermal change
Epidermal hyperplasia and a hyperpigmented basal layer were significantly more common in conventional dermatofibroma than in dermatofibroma without gross skin surface change (P < 0.001).
Tumor depth
The tumor mass of dermatofibroma without gross skin surface change was located significantly deeper (mean depth, 1.71 ±0.84 mm) than that of conventional type (0.74 ±0.31 mm, P < 0.001).
Extension to the subcutaneous layer
Although they presented clinically as a nodular lesion without gross skin surface change, histological examination revealed subcutaneous involvement in only 19 of the 42 cases of dermatofibroma without gross skin surface change. Histologically, dermal dermatofibromas with a subcutaneous extension ("deep-penetrating dermatofibroma", [Figure - 2]a and b) were found in 17 of the 42 cases (40%). Only two purely subcutaneously located dermatofibromas ("subcutaneous dermatofibroma", [Figure - 2]c and d) were noted. Except for the 19 cases of dermatofibroma with histological subcutaneous extension noted above, these dermatofibromas were located entirely within the dermis. However, subcutaneous extension was found to be significantly more common in dermatofibroma without gross skin surface change (19 (45%) of 42 cases) than in conventional type (24 (25%) of 95 cases, P = 0.020).
 |
| Figure 2: Subcutaneous extension in dermatofibroma without gross skin surface change. (a, b) "Deep-penetrating dermatofibroma" showing dermal tumor extending into the subcutaneous layer. (c, d) "Pure subcutaneous dermatofibroma" without dermal involvement (hematoxylin– Eosin stain; a, c: ×40, b, d: ×100) |
Cellular polymorphism and cellular atypia
Secondary elements, such as foam cells [Figure - 3]a and multinucleated giant cells [Figure - 3]b, were present in both dermatofibroma types, with no significant differences in numbers [Table - 1]. Cellular atypia was not a common feature, being present in only 2 (5%) of 42 dermatofibromas without gross skin surface change and 3 (3%) of 95 conventional dermatofibromas and, again, the difference was not significant (P = 0.487). There was also no significant difference in cellular mitoses between dermatofibroma without gross skin surface change (3 of 42, 7%) and conventional dermatofibroma (5 of 95, 5%).
 |
| Figure 3: Histological findings in dermatofibroma without gross skin surface change. (a) Foam cells in dermatofibroma. (b) Multinucleated giant cells in dermatofibroma. (c) Aneurysmal dermatofibroma. (d) Focal hemosiderin deposit (hematoxylin– Eosin stain; a: ×200, b: ×100, c: ×40, d: ×100) |
Variations in histology
Histological variants, i.e., cellular, aneurysmal [Figure - 3]c, and atypical dermatofibroma were found in both types of dermatofibroma with no significant differences in frequency of occurrence [Table - 1]. Focal stromal hyalinization and hemosiderin deposit were more common in the conventional type. Focal stromal hyalinization was noted in two (5%) cases of dermatofibroma without gross skin surface change and 16 (17%) cases of the conventional type (P = 0.042). This ranged from thin bands of hyalinized collagen to broad, densely collagenized areas. Focal hemosiderin deposits [Figure - 3]d were seen in two cases (5%) of dermatofibroma without gross skin surface change and 18 cases (19%) of conventional dermatofibroma (P = 0.022). Central necrosis, infarction, or cystic change was not found in any cases of dermatofibroma in the present study.
DISCUSSION
Dermatofibroma usually occurs on the extremities as reddish-brown papules or nodules, which may either be elevated or slightly depressed. Firm-hard lesions that adhere to the overlying epidermis may result in a depression over the nodule. [8] Variants of dermatofibroma can be classified into many types according to their clinical and histologic aspects. Clinical variants include atrophic, [9],[10] atypical polypoid, [11] giant, [12] subungual, [13] erosive, [14] lichenoid, [14] ulcerated [14] dermatofibroma, and grouped palmoplantar histiocytoma. [15] Several histological variants have been described, including cellular, aneurysmal, epithelioid, atypical, and myxoid, as well as "subcutaneous" and "deep-penetrating dermatofibroma". [1],[2],[3],[4],[16],[17]
"Subcutaneous variants" and "deep-penetrating dermatofibroma" are histological subtypes that involve the subcutaneous layers. [2],[3],[4] According to the World Health Organization, a deep location is seen in less than 1% of all dermatofibromas. [18] Conventional cutaneous dermatofibroma pursues a benign course with a recurrence rate of less than 2%, although higher rates of recurrence have been noted in some variants, including cellular, aneurysmal, and atypical dermatofibroma. [19] "Subcutaneous" or "deep-penetrating dermatofibromas" tend to have a higher risk of local recurrence than conventional cutaneous dermatofibroma. [3] Subcutaneous histological variants may present features not usually seen in conventional dermatofibroma, including a hemangiopericytoma-like pattern, foci of hemorrhage, increased mitotic activity, cellular atypia, and stromal anomalies such as focal hyalinization and myxoid change. [2],[3],[4] Secondary cellular elements, such as multinucleated giant cells and foam cells are commonly observed in subcutaneous histological variants. [2],[3],[4] "Purely subcutaneous dermatofibroma" is a rare histologic variant, with only two reported series of 21 and 69 cases that included dermatofibroma from both subcutaneous and deep soft tissues, such as the mediastinum and retroperitoneum. [2],[3] However, clinical features of dermatofibroma histologically located entirely within subcutaneous tissue ("pure subcutaneous dermatofibroma") were not described. The histological features of dermatofibroma clinically presenting as a subcutaneous nodular lesion without gross skin surface change have also not been described or compared with the conventional type.
Dermatofibroma without gross skin surface change is rare; the incidence of this variant was 6.3% in the present study. The lack of recognition of this variant type may result from the lack of published literature and patients being unaware of the presence of a subcutaneous nodular lesion. In this study, the age, sex, and dermatofibroma-related symptoms in patients with the two different types of dermatofibroma were not significantly different. However, interestingly, the duration of lesions was significantly longer in the conventional type than in dermatofibroma without gross skin surface change, and the frequency of size increase during the disease course was higher with conventional dermatofibroma. Dermatofibroma without gross skin surface change was more commonly located in the head and neck region than conventional type, which had a predilection for the extremities. These findings suggest that dermatofibroma without gross skin surface change is a distinct clinical variant. However, it is possible that dermatofibroma exists on a spectrum with a nodular lesion without gross skin surface change occurring at an early stage of disease and dermatofibroma with surface changes seen at a late stage of disease. Increase in tumor size at a late stage could be associated with a superficial dermal location and epidermal changes, which are findings in conventional dermatofibroma. Patients with dermatofibroma without gross skin surface change on the trunk or extremities may not visit physicians until skin surface changes develop because of the location.
The histological findings suggest that the two types of dermatofibroma, also differ in epidermal changes and subcutaneous extension. Although subcutaneous extension was more common in dermatofibroma without gross skin surface change, it was not invariable because a purely dermal location was observed in more than half of such dermatofibromas. Except for focal hyalinization and hemosiderin deposits, other particular histological features were found to the same extent in both types of dermatofibroma. Focal hyalinization and hemosiderin deposits, which were more frequent in the conventional type, could be secondary histologic changes in long-lasting dermatofibroma if a nodular lesion without gross skin surface change seen here is assumed to be an early stage in the spectrum of disease. The histological findings of dermatofibroma without gross skin surface change were different from those of subcutaneous histological variants of dermatofibroma. [2],[3],[4] Histological characteristics of subcutaneous histological variants (a hemangiopericytoma-like pattern, increased mitotic activity, cellular atypia, and secondary cellular elements) were not common in these dermatofibromas. Mentzel et al. [20] reported that dermatofibroma on the face could not easily be clinically suspected because it presents unusual features such as ill-defined lesions with infiltration of deeper structures. Dermatofibroma on the face had unusual histological findings characterized by subcutaneous extension, cellular fascicles, bundles of spindle-shaped tumor cells, and increased atypia. [20] Although dermatofibromas without gross skin surface change in this study were commonly located in the head and neck region, the unusual histological findings described for dermatofibroma on the face were not found. Most dermatofibromas on the face were not entirely confined to the dermis, [20] whereas a purely dermal location was observed in more than half of dermatofibroma without gross skin surface change in our present study.
This study shows that dermatofibroma without gross skin surface change, clinically and histologically differs from the conventional type. To elucidate the morphological and histological changes during the disease course of dermatofibroma, additional multicenter, prospective studies that include serial histologic features are needed. Clinical differences in duration of disease and change in size during the disease course suggest that subcutaneous nodular lesion without gross skin surface change could represent an early stage in the disease progression of dermatofibromas.
| 1. |
Calonje E, Fletcher CD. Cutaneous fibrohistiocytic tumors: An update. Adv Anat Pathol 1994;1:2-15.
[Google Scholar]
|
| 2. |
Fletcher CD. Benign fibrous histiocytoma of subcutaneous and deep soft tissue: A clinicopathologic analysis of 21 cases. Am J Surg Pathol 1990;14:801-9.
[Google Scholar]
|
| 3. |
Gleason BC, Fletcher CD. Deep "benign" fibrous histocytoma: Clinicopathologic analysis of 69 cases of a rare tumor indicating occasional metastatic potential. Am J Surg Pathol 2008;32:354-62.
[Google Scholar]
|
| 4. |
Kamino H, Jacobson M. Dermatofibroma extending into the subcutaneous tissue. Differential diagnosis from dermatofibrosarcoma protuberans. Am J Surg Pathol 1990;12:1156-64.
[Google Scholar]
|
| 5. |
Wick MR, Ritter JH, Lind AC, Swanson PE. The pathological distinction between "deep penetrating" dermatofibroma and dermatofibrosarcoma protuberans. Semin Cutan Med Surg 1999;18:91-8.
[Google Scholar]
|
| 6. |
Ito T, Yoshida Y, Furue M, Yamamoto O. Subcutaneous benign fibrous histiocytoma showing nerve involvement on the eyebrow region. Acta Derm Venereol 2013;93:371-2.
[Google Scholar]
|
| 7. |
Franquemont DW, Cooper PH, Shmookler BM, Wick MR. Benign fibrous histiocytoma of the skin with potential for local recurrence: A tumor to be distinguished from dermatofibroma. Mod Pathol 1990;3:158-63.
[Google Scholar]
|
| 8. |
James WD, Berger TG, Elston DM. Dermal and subcutaneous tumors. In: Andrews' diseases of the skin, Clinical dermatology, 10 th ed. Philadelphia: SAUNDER; 2006. p. 611-2.
th ed. Philadelphia: SAUNDER; 2006. p. 611-2.'>[Google Scholar]
|
| 9. |
Chang SE, Choi JH, Sung KJ, Moon KC, Koh JK. Subcutaneous dermatofibroma showing a depressed surface. Int J Dermatol 2001;40:77-8.
[Google Scholar]
|
| 10. |
Hendi A, Jukic DM, Kress DW, Brodland DG. Atrophic dermatofibroma: A case report and review of the literature. Dermatol Surg 2002;28:1085-7.
[Google Scholar]
|
| 11. |
Puig L, Esquius J, Fernández-Figueras MT, Moreno A, de Moragas JM. Atypical polypoid dermatofibroma: Report of two cases. J Am Acad Dermatol 1991;24:561-5.
[Google Scholar]
|
| 12. |
Requena L, Fariña MC, Fuente C, Piqué E, Olivares M, Martín L, et al. Giant dermatofibroma: A little-known clinical variant of dermatofibroma. J Am Acad Dermatol 1994;30:714-8.
[Google Scholar]
|
| 13. |
Baran R, Perrin C, Baudet J, Requena L. Clinical and histological patterns of dermatofibromas of the nail apparatus. Clin Exp Dermatol 1994;19:31-5.
[Google Scholar]
|
| 14. |
Sánchez Yus E, Soria L, de Eusebio E, Requena L. Lichenoid, erosive and ulcerated dermatofibromas. Three clinico-pathologic variants. J Cutan Pathol 2000;27:112-7.
[Google Scholar]
|
| 15. |
Bedi TR, Pandhi RK, Bhutani LK. Multiple palmoplantar histiocytomas. Arch Dermatol 1976;112:1001-3.
[Google Scholar]
|
| 16. |
Zelger BG, Calonje E, Zelger B. Myxoid dermatofibroma. Histopathology 1999;34:357-64.
[Google Scholar]
|
| 17. |
De Hertogh G, Bergmans G, Molderez C, Sciot R. Cutaneous cellular fibrous histiocytoma metastasizing to the lungs. Histopathology 2002;41:85-6.
[Google Scholar]
|
| 18. |
Garrido-Ruiz MC, Ramos P, Enguita AB, Rodriguez Peralto JL. Subcutaneous atypical fibrous histiocytoma. Am J Dermatopathol 2009;31:499-501.
[Google Scholar]
|
| 19. |
Bisceglia M, Attino V, Bacchi CE. Metastasizing "benign"fibrous histiocytoma of the skin: A report of two additional cases and review of the literature. Adv Anat Pathol 2006;13:89-96.
[Google Scholar]
|
| 20. |
Mentzel T, Kutzner H, Rütten A, Hügel H. Benign fibrous histiocytoma (dermatofibroma) of the face: Clinicopathologic and immunohistochemical study of 34 cases associated with an aggressive clinical course. Am J Dermatopathol 2001;23:419-26.
[Google Scholar]
|
Fulltext Views
4,902
PDF downloads
1,202





