Translate this page into:
Role of nail biopsy as a diagnostic tool
2 Department of Pathology, Maulana Azad Medical College, New Delhi, India
3 Department of Dermatology, Venereology, and Leprology, Mamata Medical College, Khammam, AP, India
Correspondence Address:
Chander Grover
420 B, DDA Flats, Pocket II, Mayur Vihar Phase I, Delhi 110 091
India
| How to cite this article: Grover C, Chaturvedi UK, Reddy BN. Role of nail biopsy as a diagnostic tool. Indian J Dermatol Venereol Leprol 2012;78:290-298 |
Abstract
Nail biopsy (NB) is an investigation that is not routinely resorted to by most of the dermatologists. The commonly cited reasons are the complexity of the procedure, risk of scarring and the reluctance of the patient. However, in cases with isolated nail psoriasis, isolated nail lichen planus, onychomycosis not confirmed on direct microscopy and culture, or longitudinal melanonychia, the treating dermatologist is left with no choice but to resort to this procedure. Nail as a unit, is capable of projecting only a limited number of clinical manifestations. This is responsible for the more or less similar clinical presentation of many different nail disorders. Hence, a practical knowledge of the indications, appropriate patient selection, procedural details and histopathological interpretation of a NB is a must-have for any practicing dermatologist. The risk of scarring is none to minimal if appropriate type of biopsy is performed, not to mention the wealth of histopathological data that can be retrieved from the nail unit. This article aims to explore the various practical do's and don'ts for the NB and tells us what to expect from of the procedure.Introduction
The nail biopsy (NB) is a useful technique to obtain a diagnosis of a clinically ambiguous nail condition that is not diagnosable by history, clinical appearance and routine mycology. [1] It is an investigation that not only provides etiologic, diagnostic and prognostic information but also aids in understanding the pathogenesis of nail diseases. [2] No doubt it is of great academic value, but the question addressed in this manuscript is the practical utility of NB in our day to day dermatologic practice. This article is not aimed at teaching the NB techniques in great detail but at putting forth practical tips, do′s and don′ts with respect to a NB.
For years, NB has been shunned as a difficult and scarring procedure, which is seldom required in day to day practice. [2] Only a few studies with a limited number of patients have been carried out to assess the utility of NB in dermatology, [2],[3],[4],[5] while some others have focussed on histopathology of specific nail diseases, e.g. onychomycosis, [6],[7] psoriasis, [4],[8] melanonychia, [9],[10] etc. Apart from these attempts, NB and nail histopathology have not been in much vogue either in the literature or in practice due to various factors. The objective of a NB is to arrive at a precise diagnosis of nail pathology with a simple, safe surgical procedure, simultaneously avoiding pain or permanent nail dystrophy. [1] Not every patient needs to undergo NB but, when required, there are certain essential prerequisites to be fulfilled.
Prerequisites for A Nail Biopsy
Knowledge of nail anatomy
A precise understanding of the nail anatomy is an essential prerequisite, and one can refer to standard texts on this subject as it is out of scope of the present communication. [1],[11] While operating, the nail unit anatomy should be thoroughly respected. The essential structures like the ventral and proximal nail matrix (responsible for nail plate surface), the distal nail matrix (responsible for nail plate structure and adherence to nail bed), and the extensor tendons (responsible for normal movement and function) of the digit should be safeguarded. Because of the absence of any subcutaneous tissue in the nail unit, any biopsy of the nail unit needs to be taken down to the periosteum.
Patient selection
Patient selection is important as NB needs to be performed only for a patient in whom the diagnosis has not been forthcoming due to the absence of typical skin lesions or histopathology and the nail condition does not yield adequate information on routine investigations like direct microscopy or culture. An ideal candidate for NB should be the one in whom either there are no skin lesions or they are not contributing towards a diagnosis, as skin biopsy is always a safer and easier procedure than NB. Patients with diabetes, peripheral vascular disease, or arterial insufficiency should not be subjected to NB. [12] An informed written consent should be taken as with all other surgical procedures.
Surgical technique
Exsanguination followed by a digital tourniquet is also an essential prerequisite for any fruitful procedure, as the nail bed is a highly vascular structure that may bleed profusely when manipulated. It is important to note that the tourniquet should not be kept on for more than 15 min at a stretch. [1] Commonly used nail unit anesthesia techniques include the proximal "ring block" (infiltration of anesthetic solution at the base of the digit) or the distal "wing block" (infiltration in the proximal and lateral nail folds). [1]
Instrumentation
Appropriate instruments make life easy for any nail surgeon. The nail spatula/elevator, nail splitter, and sharp biopsy punches (3 mm and 4 mm) are absolute must haves for a nail surgeon. Skin hook, fine-tipped, curved atraumatic forceps and scissors are valuable add-ons [Figure - 1].
 |
| Figure 1: Instruments required for a nail biopsy. Shown are fine curved (Castro Veijo's) scissors, fine curved (Jeweller's) forceps, nail spatula, nail splitter, and disposable biopsy punches (3 mm and 4 mm) |
Histopathology
A competent dermatopathologist who is familiar with the basic histopathologic features of the nail is also an essential prerequisite. It is important to note that there are basic differences in nail histopathology in health as well as in disease, as compared to that of the skin, and these need to be understood and appreciated. [13] Proper embedding and sectioning of the NB specimen is essential prior to this.
Side-effects
The risks associated with the NB procedure should be explained and consent of the patient must be obtained beforehand. These include the possibility of permanent nail dystrophy, possibility of not achieving a diagnosis even after NB, more time required for regrowth of the nail, bleeding, and risk of infection as with any other surgery.
Techniques/Types
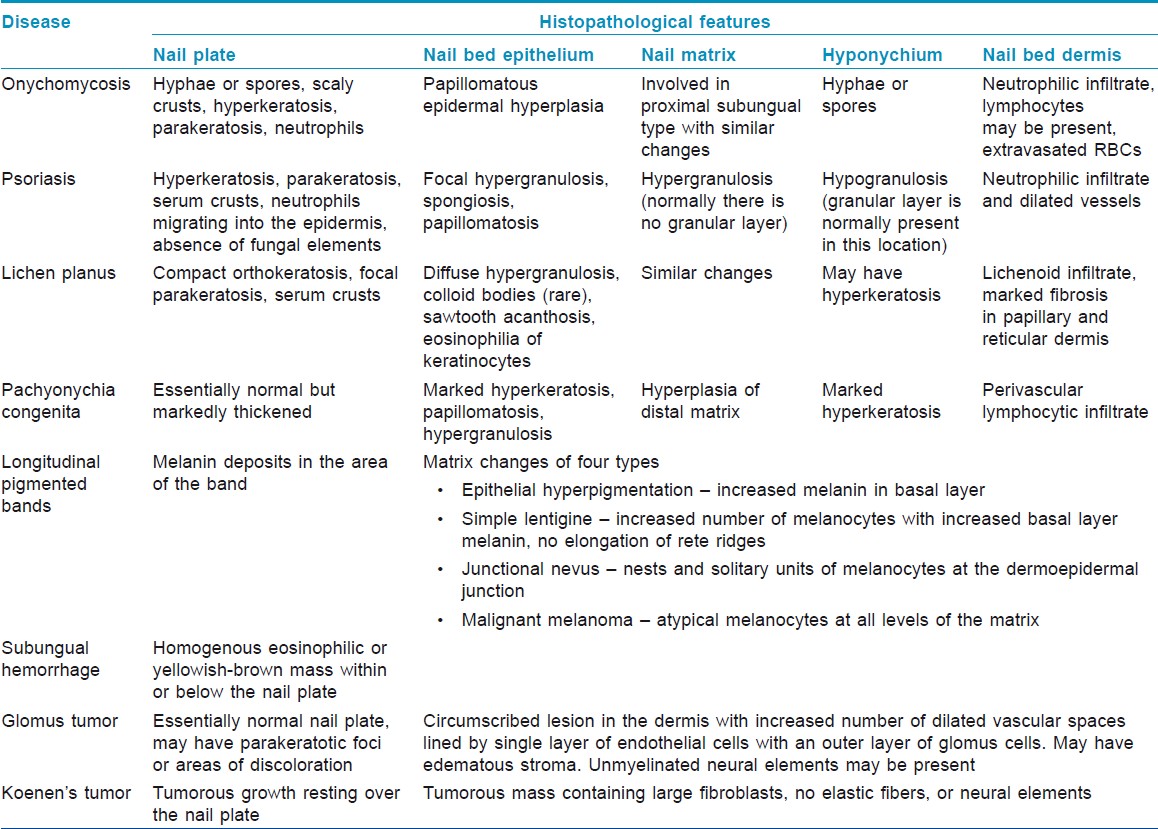
NB could be taken as an excision biopsy, punch biopsy, or longitudinal biopsy. A punch or an excision biopsy can be applied to any individual anatomical part of the nail unit, like the nail bed, nail plate, nail fold, or matrix. A longitudinal NB gives maximum histopathological information, but it is not routinely resorted to due to its scarring potential. Nail as a unit is capable of producing a very limited set of clinical reaction patterns, e.g. onycholysis can be a manifestation of onychomycosis, nail psoriasis, or even nail lichen planus. Hence, finding a histopathologic cause is generally required prior to initiating specific therapy. The trick lies in choosing the area to be biopsied, i.e. the area that will show the histopathological diagnostic changes, and [Table - 1] can serve as a guide in this regard. As is well known, the changes in nail plate occur as a result of the pathology of the nail matrix; hence, the histopathological features of disorders like melanonychia, erythronychia, pitting, etc. are best represented in a nail matrix biopsy. However, for features like onycholysis, subungual hyperkeratosis, salmon patch, etc. one would need to take a nail bed biopsy.
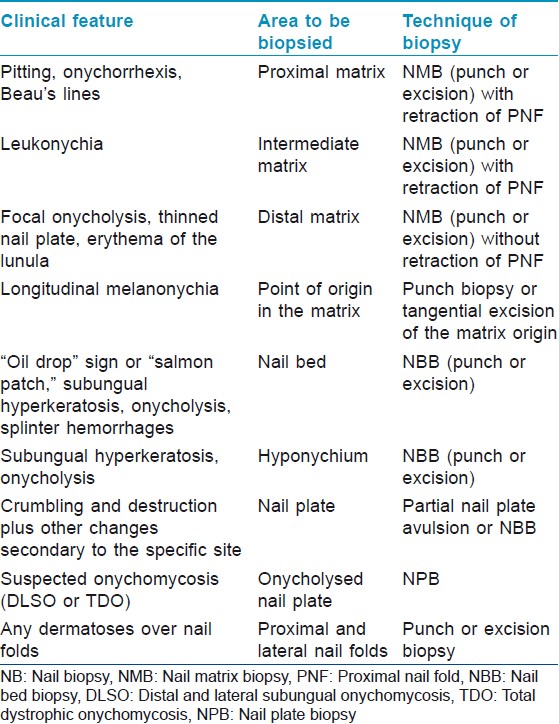
Based on the site from where it is being taken, NB can be classified as follows [Figure - 2]:
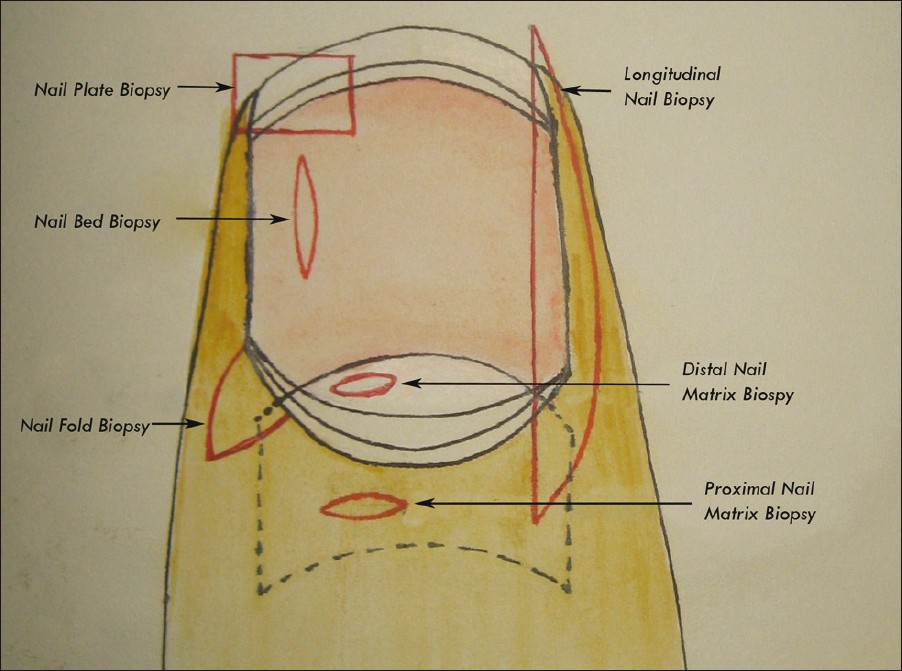 |
| Figure 2: Different types of nail biopsy. The incision lines are shown in red |
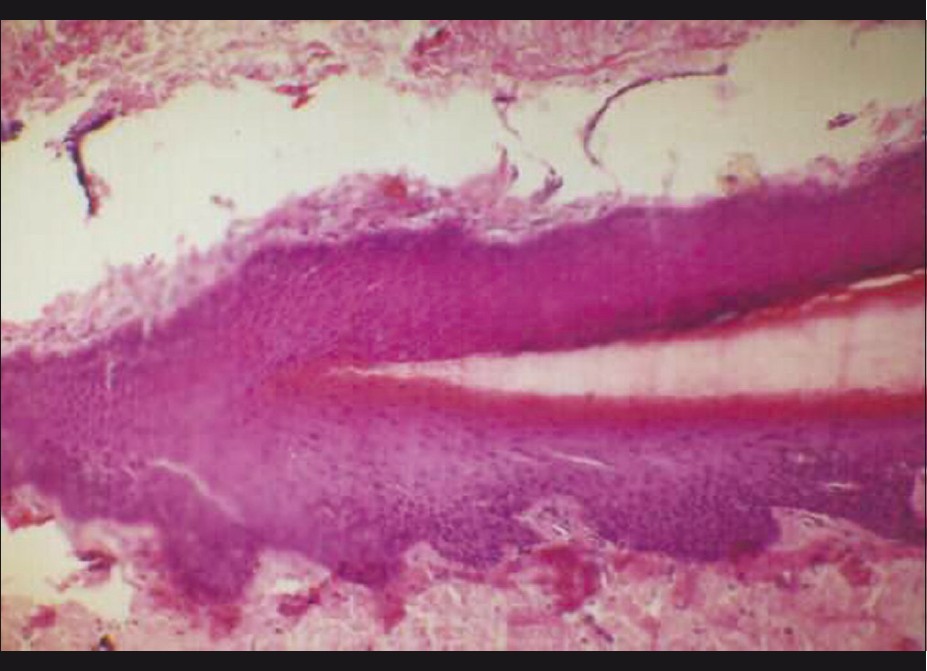
- Nail plate biopsy (NPB) is the easiest and the least-scarring technique, wherein a part of the nail plate (onycholysed or not) is separated and sent for histopathologic analysis. [7] It gives limited histopathological data but is useful in suspected cases of onychomycosis (demonstrates nail plate fungal invasion), [7] warts (adherent epithelium will show koilocytes [2] ) [Figure - 3], and also nail psoriasis (nail plate neutrophilic infiltration, serum crusts, and parakeratosis can be easily seen). The utility of NPB in systemic disease has also been explored extensively. [14]
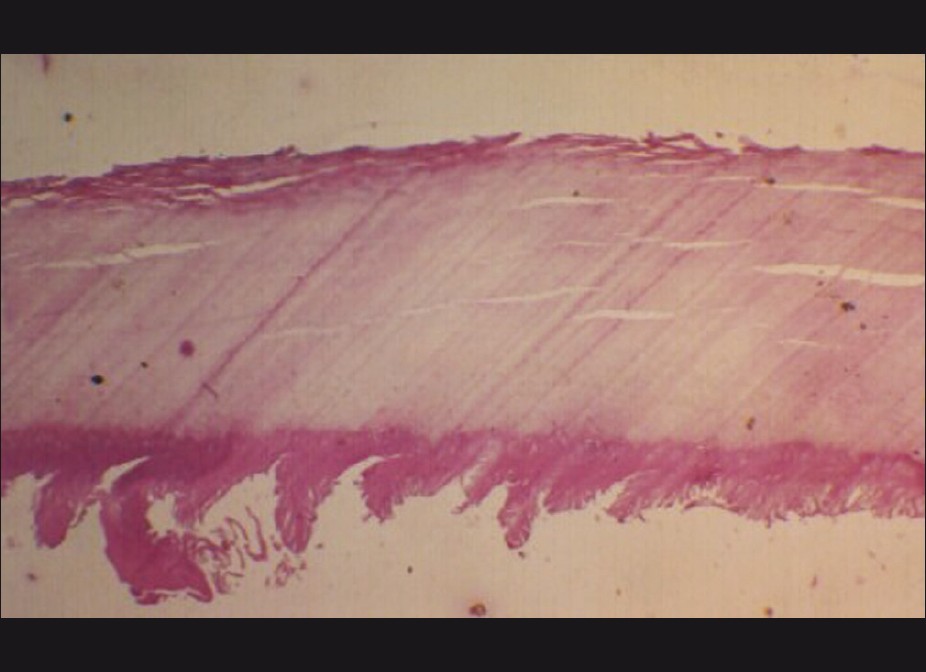
Figure 3: Nail plate biopsy with adherent nail plate epithelium showing evidence of a subungual wart. Note the marked papillomatosis of the nail bed epithelium (H and E, ×60) - Nail bed biopsy (NBB) is generally performed to distinguish between two or more conditions with a similar clinical pattern, like onycholysis or subungual hyperkeratosis, cases with discoloration of the nail bed, or any painful nail bed lesion. It can be an elliptical excision (longitudinally oriented) or a punch biopsy [Figure - 4]. Prior nail avulsion may or may not be required. If required, then partial avulsion to expose the area to be biopsied is preferred to total avulsion. Nail bed defects up to 3 mm can be left unsutured. [1],[12] Postoperative healing of the nail bed is generally uneventful, and the incidence of scarring and onycholysis is low. NBB is of therapeutic utility in cases with nail bed tumors, like glomus tumor.

Figure 4: Procedure of a nail bed biopsy. (a) Suspected nail bed glomus tumor. (b) Subungual glomus tumor seen as a bluish mass after nail plate avulsion. (c) Excision of the tumor done. Note that the nail bed incisions are oriented longitudinally. (d) Defect >3 mm in width needs to be sutured - Nail fold biopsy (NFB) can be done from the proximal (PNF) or lateral nail fold (LNF), and is indicated for paronychial dermatoses, inflammation, or nail fold tumors (benign or malignant). It can be shave biopsy, elliptical excision, punch, or en bloc excision (for PNF). [15] Prior to any excision over the nail folds, it is wise to insert a nail spatula underneath the concerned fold to prevent any inadvertent damage to the underlying nail bed or matrix.
- Nail matrix biopsy (NMB) is resorted to for the exploration of matrix origin of longitudinal pigmented bands, benign lesions of the nail matrix (glomus tumor), malignant lesions (melanoma), or acquired nail plate defects like punctate leukonychia, onychorrhexis, or pitting. The techniques employed are elliptical excision (horizontally oriented), punch excision (≤3 mm), and tangential (shave) excision. A proximal nail fold-lunula double-punch technique has also been described. [16] Whenever possible, the distal matrix should be biopsied rather than the proximal matrix, and the lunular margin should not be compromised to minimize scarring. If a biopsy is to be taken from the proximal matrix, lateral release incisions at the junction of proximal and lateral nail folds along with stay sutures (as shown) help in exposing the proximal matrix area [Figure - 5].

Figure 5: Procedure of nail matrix biopsy. For adequate exposure of the proximal matrix, lateral incisions are made at the junction of the proximal and lateral nail folds. The proximal nail fold is then lifted up and retracted with the help of stay sutures. An adequate - sized punch is then driven down up to the periosteum and the punch biopsy specimen is lifted up - Longitudinal nail biopsy (LNB) is performed when it is desirable to sample the entire nail unit. [17],[18] The resultant defect needs to be sutured to ensure proper healing [Figure - 6]. It is a very useful technique for the treatment of larger lesions placed asymmetrically over the affected nail. This technique samples the representative areas of each part of the nail unit, and has been of immense academic help. However, being a potentially scarring procedure, its utility in day to day clinical practice is low.
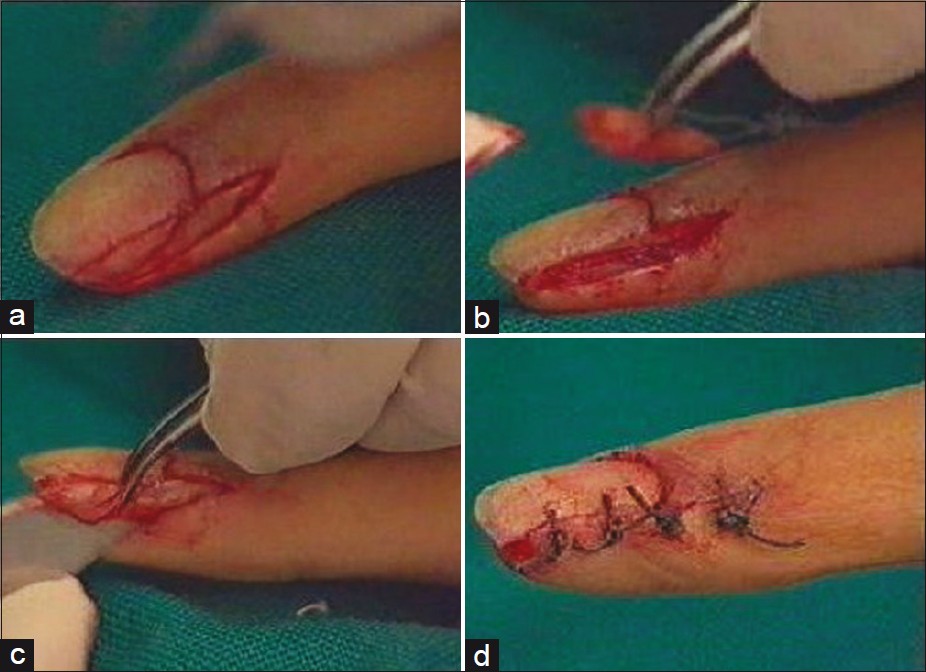
Figure 6: Procedure of longitudinal nail biopsy. (a) The area to be excised is outlined. The incision is linear medially and curved laterally. (b) The incision is carried down to the periosteum and the tissue is lifted up with sharp dissection. (c) The separated specimen for histopathologic examination. (d) The defect is sutured back
Nail plate specimens when taken as a part of biopsy need to be softened before processing. For this purpose, various agents have been recommended, which include 3% phenol, cedar wood oil, and chitin-softening solutions composed of mercuric chloride, chromic acid, acetic acid, and 95% alcohol. [2]
Complications expected with the NB include bleeding, secondary infection, scarring of nail bed, onycholysis, and reduction in nail width, malalignment of the axis of the regrowing nail, or growth of nail spicules. [12] The last three are almost exclusively seen with LNB .
Histopathology
The nail unit has few histopathological features distinct from the normal skin [13] [Figure - 7]. Nail fold epithelium lacks any pilosebaceous units, and rete ridges are also minimal to absent. Nail matrix epithelium has broad, club-shaped rete ridges pointing proximally. It is devoid of a granular layer and undergoes onychokeratinisation to produce the nail plate. There is a high density of melanocytes seen even in layers above the basal layer. Nail plate is composed of cornified cells without nuclei, arranged in lamellae that stain strongly with acid fast stains. Nail bed epithelium is only two to three layers thick, devoid of a granular layer, and lacks rete ridges in a sagittal section. The granular layer reappears in the epithelium of the hyponychium. The dermis is highly vascular, containing numerous nerve endings, specialized nerve structures, and glomus bodies.
 |
| Figure 7: Normal nail unit histopathology showing the nail matrix area. The nail plate is seen arising over the nail matrix area. The characteristic absence of granular layer in the nail matrix epithelium can be noted (H and E, ×160) |
Not surprisingly, the nail unit histopathology features in disease are also quite different, e.g. in contrast to skin psoriasis, nail psoriasis is characterized by hypergranulosis. The salient features of nail histopathology in selected diseases are outlined in [Table - 2]. [2],[4],[13] One fact to be borne in mind is that the thin nail bed epithelium is tightly adherent to the nail plate and tends to get avulsed along with it. Hence, a NBB performed after avulsing the nail plate may not give adequate histopathological information, especially in case of inflammatory nail pathology (personal observation) [Figure - 3].
Indications
Earlier studies have described varying degrees of success in establishing a diagnosis with NB. Hanno et al. studied predominantly inflammatory nail pathologies and found diagnostic features in 40% of their cases. [4] In the series by de Berker et al. comprising mainly of tumors, 93.93% biopsies were diagnostic. [5] Grover et al. evaluated 60 nail biopsies of infective as well as noninfective disorders, and found diagnostic histopathology in 64% cases. [2] NB was reported especially useful for definitive diagnosis in nail tumors and infections. [2],[4],[5] All these studies have documented a low risk of side-effects to NB and demonstrated it to be a simple and safe procedure. [2],[7],[12] A skillfully performed adequate NB, handled, processed, and interpreted properly, can be an important part of the dermatologist′s armamentarium in providing excellent, comprehensive patient care. [19]
The utility of various types of NB has been studied extensively for various common and uncommon nail disorders.
Onychomycosis
This has been an area of active research, [6],[7],[20],[21] and NB with PAS staining has been reported to be the most sensitive method for diagnosis [6] [Figure - 8]. Routine histological examination with PAS staining before initiating antifungal therapy was recommended initially. [21] However, in later studies, histopathologic examination has been proposed as a useful complimentary test, indicated if results of other methods are negative and clinical suspicion is high. [6],[7]
 |
| Figure 8: Fungal pseudohyphae seen in a nail plate biopsy (H and E, ×400) |
Twenty nail dystrophy
NB has revealed that the disorder Twenty nail dystrophy (TND) is multifactorial in origin as it may show histopathologic features of nail psoriasis, lichen planus, or spongisosis. [18],[22],[23],[24] NB has a definite diagnostic utility in cases with TND, where the clinical diagnosis is obscure because of the absence of cutaneous associations. However, it cannot be recommended for the routine evaluation of this otherwise benign disorder, especially because the further treatment options are generally not altered. [25]
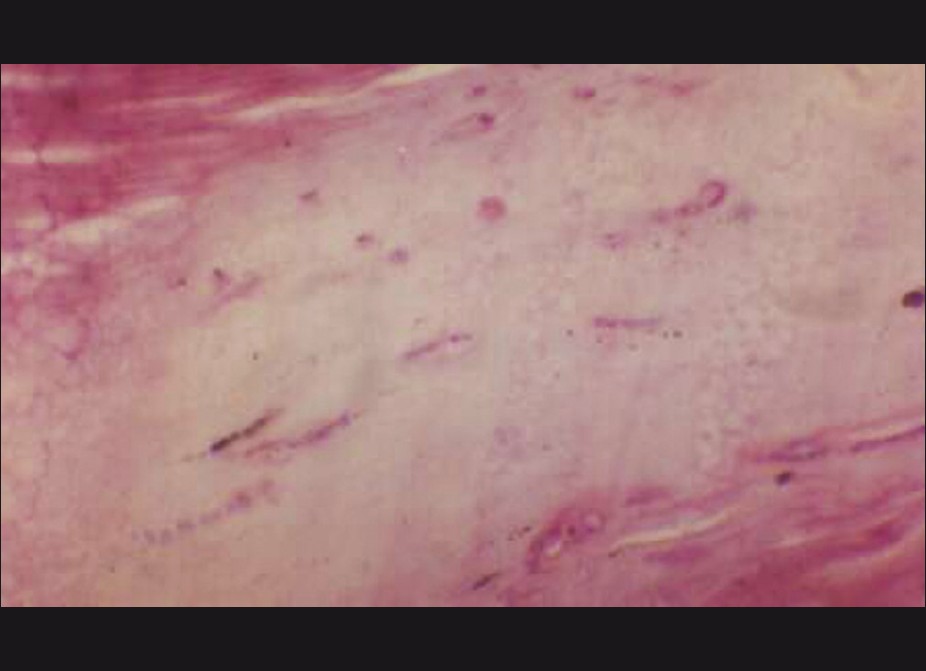
Nail psoriasis
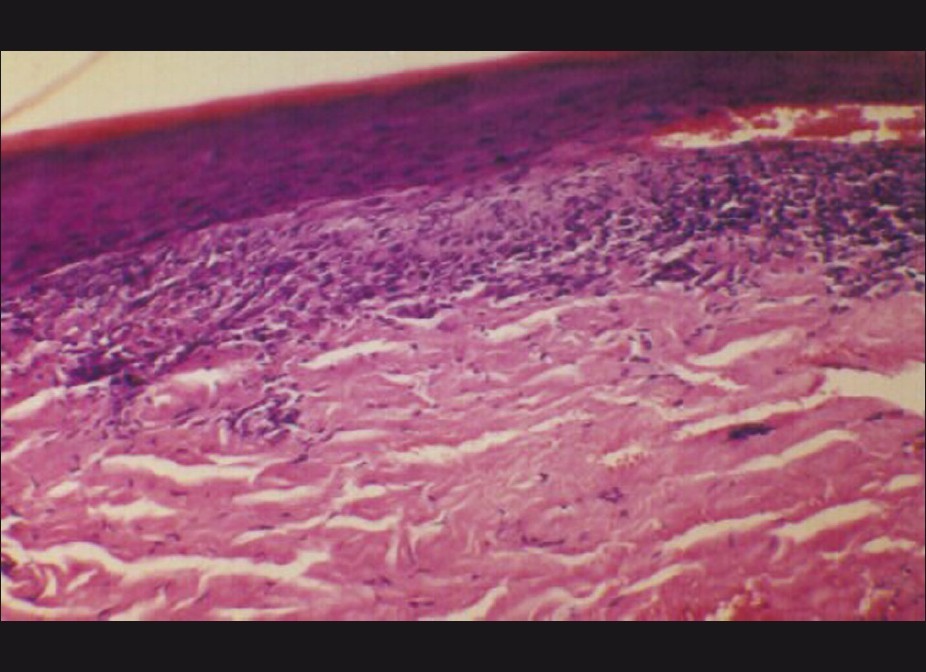
NB for nail psoriasis has been an area of interest, especially because 1-5% of the cases with psoriasis may present with purely nail manifestations only. [8] Hanno et al. proposed diagnostic criteria of nail psoriasis in the form of presence of neutrophils in the nail bed epithelium (major criterion), hyperkeratosis with parakeratosis, serum exudates, focal hypergranulosis, and nail bed epithelium hyperplasia (minor criteria) [4] [Figure - 9]. As onychomycosis may show similar features, Grover et al. suggested that PAS negativity for fungal hyphae should be included as a major criterion for the diagnosis of nail psoriasis. [8]
 |
| Figure 9: Nail unit biopsy showing psoriasis. Hypergranulosis, parakeratosis, parakeratotic abscess, and serum crusting can be appreciated (H and E, ×160) |
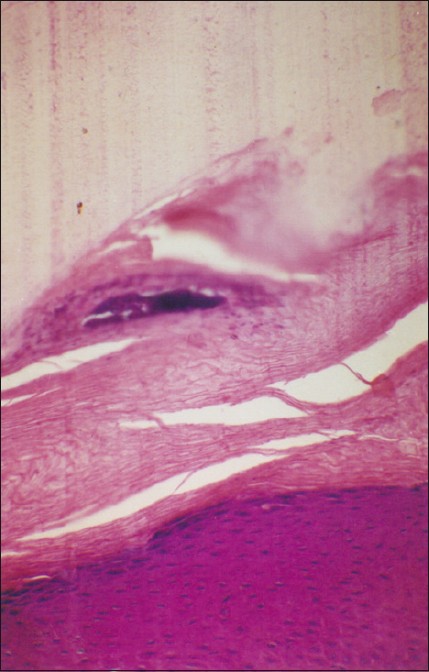
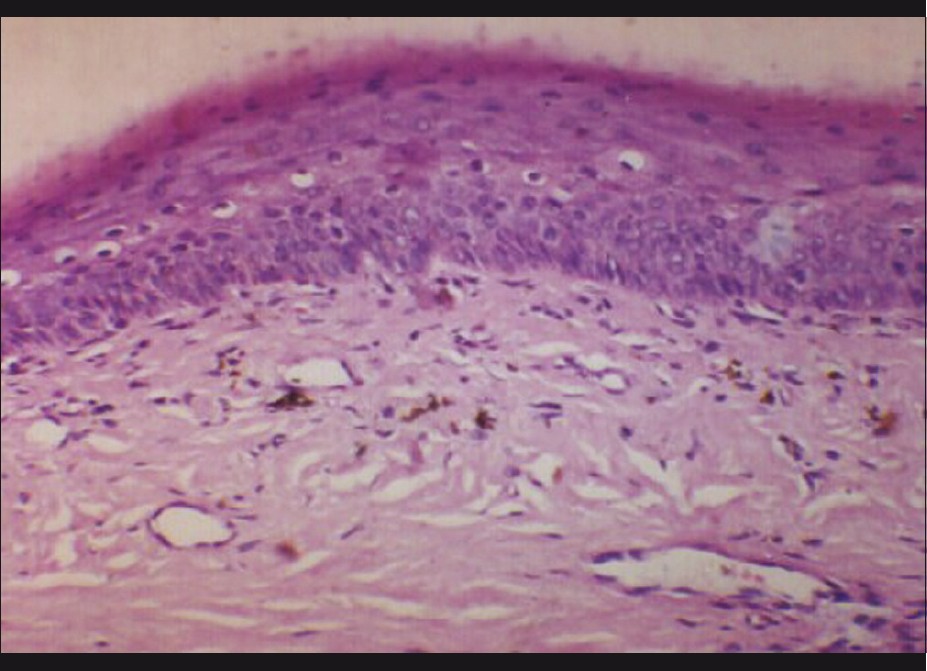
Nail lichen planus
Isolated nail lichen planus (LP) comprises 1-10% cases of LP. As nail LP is potentially scarring and the changes may be irreversible, an effective management of the condition requires that the diagnosis be confirmed on histopathology. The diagnostic features of nail LP have been described on NB. [4],[26],[27] Peluso et al. reported the utility of NB in confirming the diagnosis of LP in an 11-year-old boy, which enabled successful treatment of the case [27] [Figure - 10].
 |
| Figure 10: Nail bed epithelium showing changes suggestive of lichen planus. Basal layer dissolution and a band-like infiltrate hugging the epidermis can be seen (H and E, ×160) |
Other dermatoses
NB has been useful in establishing diagnosis in isolated nail lichen striatus [28] and sarcoidosis. [29] However, in PRP, the nail histopathological changes represent a nonspecific reaction pattern and are not diagnostic. [30] The ultrastructural studies of NPB have also been reported to be a useful diagnostic tool in distinguishing lamellar ichthyosis from other ichthyoses, with overlapping clinical features. [31]
Melanonychia
NB is of particular use in the evaluation of pigmented nails, especially longitudinal melanonychia. [9],[10] Histopathologically, the matrix lesion responsible for pigmented nail bands may be of four types [9] [Table - 2]. Epidermal hyperpigmentation represents melanocyte activation due to inflammation, trauma, friction, or drugs [Figure - 11]. Nail matrix may also have a simple lentigene or nail matrix nevus. However, the most ominous diagnosis is that of a malignant melanoma that can be effectively ruled out with a NB. Tosti et al. studied nail matrix nevi histologically in 22 patients and reported that a diagnosis of nail matrix nevus is impossible clinically and always requires histopathologic study. Further, nail matrix nevi resemble skin nevi histopathologically except for their architectural pattern, which reflects the peculiar anatomy of the nail unit. [9]
 |
| Figure 11: Nail matrix biopsy from the case shown in Figure 5, showing pigment - laden cells in dermis-melanocyte activation (H and E, ×250) |
Tumors
Nail matrix is the most common site for Glomus tumor, and excision biopsy provides treatment, relief from pain, and histological diagnosis in one go [32] [Figure - 4]. Periungual fibromas are benign tumors that are a cutaneous manifestation of tuberous sclerosis complex. They can bleed, cause pain, and distort the nail. Their histopathologic features have been studied in detail by Ma et al. [33] Squamous cell carcinoma is the other malignancy common in the nail bed that can be diagnosed easily with a NB. [34],[35]
Systemic diseases
NB (especially NPB) has also been reported to be useful in the study of systemic diseases. Tirado-Gonzalez et al. proposed that fluids exude or transude into nail structures providing a kind of ′′nail window′′ into systemic hematologic or metabolic abnormalities. [14] Detection of urate crystals in the subungual horn of nails submitted for a suspected diagnosis of onychomycosis has been reported. [14] It is even proposed that gout may be monitored by means of the simple and noninvasive histological processing of nail clippings. However, for proper evaluation of the character of such crystals, nail plate specimens need to be submitted in alcohol rather than in formaldehyde. The presence of characteristic cytologic and histologic findings in a nail plate biopsy can expand the armamentarium of physicians to evaluate nail diseases and even systemic diseases in a noninvasive manner. [14] Bolliger et al. determined the urea, ammonia, and uric acid content of toenails in 11 patients with varying types and degrees of renal impairment and found a markedly elevated content of uric acid in patients with chronic nephritis and with long-standing severe gout. [36]
Pros and Cons of Nail Biopsy
From the aforementioned discussion, it is clear that NB offers certain special advantages. NB, especially NPB, is a relatively easy procedure, least traumatic, and can be done easily. It is seldom scarring except for the more radical LNB, which, anyhow, is not routinely resorted to by most of the dermatologists. NB is of utmost value in cases where no cutaneous changes are present, e.g. isolated nail psoriasis or nail lichen planus or other isolated nail dystrophies due to obscure dermatoses as described earlier. Hence, all of us need to train ourselves to be able to perform NB and reach a conclusion rather than initiating therapy on the basis of conjectures [Table - 3].
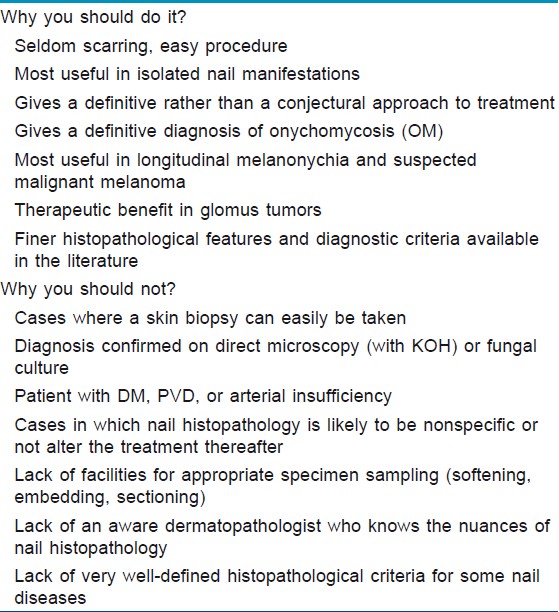
NB provides a definitive diagnosis in onychomycosis as it reveals conclusive evidence of nail plate invasion by the fungus, besides effectively differentiating the cases with secondary contamination of subungual debris of dystrophic nails. The conventional techniques of direct microscopy and culture for mycotic elements may give a false-positive report in such cases, due to which unnecessary and unsuccessful treatment may be resorted to. NB is also the single most sensitive technique of these three procedures. [6] In addition, an expert dermatopathologist can also differentiate between dermatophytes and NDM on routine histopathology thus giving valuable information regarding the choice of appropriate drug. [37] Poor growth rates on fungal culture means that this information is generally not available to the treating dermatologist.
In cases with melanonychia, NB is the only investigation that can give any answers, especially when melanoma is suspected. Excision NBB is of therapeutic benefit in nail tumors, especially the glomus tumor. In TND, NB is the only technique that can guide toward the underlying condition responsible.
However, there are certain inherent disadvantages as well. The procedure should not be attempted without a proper knowledge of nail unit anatomy, especially the matrix area. Attention to surgical technique, including proper anesthesia, is a must for achieving desirable outcomes. Experience goes a long way in improving the diagnostic yield and minimizing the associated procedural side-effects. The risk of long-term nail scarring if surgical technique is not proper and the risk of secondary infection, especially in a tropical country like ours, is to be taken care of. Also, one should be able to choose the representative area that will yield the best diagnostic information. An essential requirement is an efficient dermatopathologist well versed in the interpretation of normal and abnormal nail histology as there are many differences as compared with the normal and abnormal skin histology. A properly processed sample with a softened nail plate enables cutting of good sections under a microtome, minimizing any cutting artefacts.
Current knowledge about the histopathological details on nail specimens is limited, especially in relation to the uncommon nail disorders. The diagnostic criteria for some common diseases like nail psoriasis and lichen planus are constantly being improved upon. Perhaps, this could partly be due to the reluctance of dermatologists towards obtaining a NB for diagnostic purposes, thereby resulting in the scarcity of NB specimens reaching pathology laboratories and curtailing the experience of pathologists in the field of histological interpretation of NB.
Conclusion
A NB is not indicated for each and every disorder manifesting in the nail unit. However, when it is indicated, it is often the only clue left to achieve a diagnosis. Hence, a practicing dermatologist cannot afford to be unaware of or untrained in the technique of obtaining NB. Further, pathologists need to be trained in interpreting nail specimens, as the histopathological outcome can only be improved with more familiarity, assessment of specimens, and refinement of diagnostic criteria. The more the specimens are seen, the more details and refinements will emerge. With increased detailing, proper orientation and sectioning, sophisticated microtomes, and staining procedures, a wealth of information awaits us in the humble nail.
| 1. |
Rich P. Nail biopsy: Indications and methods. Dermatol Surg 2001;27:229-34.
[Google Scholar]
|
| 2. |
Grover C, Nanda S, Reddy BS, Chaturvedi KU. Nail biopsy: Assessment of indications and outcome. Dermatol Surg 2005;31:190-4.
[Google Scholar]
|
| 3. |
Barrera-Vigo MV, Tejera-Vaquerizo A, Mendiola-Fernández M, Cid J, Cabra-de Luna B, Herrera-Ceballos E. Diagnostic utility of nail biopsy: A study of 15 cases. Actas Dermosifiliogr 2008;99:621-7.
[Google Scholar]
|
| 4. |
Hanno R, Mathes BM, Krull EA. Longitudinal nail biopsy in evaluation of acquired nail dystrophies. J Am Acad Dermatol 1986;14:803-9.
[Google Scholar]
|
| 5. |
de Berker DA, Dahl MG, Comaish JS, Lawrence CM. Nail surgery: An assessment of indications and outcome. Acta Derm Venereol 1996;76:484-7.
[Google Scholar]
|
| 6. |
Weinberg JM, Koestenblatt EK, Jennings MB. Utility of histopathologic analysis in the evaluation of onychomycosis. J Am Podiatr Med Assoc 2005;95:258-63.
[Google Scholar]
|
| 7. |
Grover C, Reddy BS, Chaturvedi KU. Onychomycosis and the diagnostic significance of nail biopsy. J Dermatol 2003;30:116-22.
[Google Scholar]
|
| 8. |
Grover C, Reddy BS, Uma Chaturvedi K. Diagnosis of nail psoriasis: Importance of biopsy and histopathology. Br J Dermatol 2005;153:1153-8.
[Google Scholar]
|
| 9. |
Tosti A, Baran R, Piraccini BM, Cameli N, Fanti PA. Nail matrix nevi: A clinical and histopathologic study of twenty-two patients. J Am Acad Dermatol 1996;34:765-71.
[Google Scholar]
|
| 10. |
Goettmann-Bonvallot S, André J, Belaich S. Longitudinal melanonychia in children: A clinical and histopathologic study of 40 cases. J Am Acad Dermatol 1999;41:17-22.
[Google Scholar]
|
| 11. |
deBerker DA, Baran R, Dawber RP. Disorders of nails. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 7 th ed, Massachusetts: Blackwell Publishing; 2004. p 62.1-8.
th ed, Massachusetts: Blackwell Publishing; 2004. p 62.1-8.'>[Google Scholar]
|
| 12. |
Moossavi M, Scher RK. Complications of nail surgery: A review of the literature. Dermatol Surg 2001;27:225-8.
[Google Scholar]
|
| 13. |
Jerasutus S. Histopathology. In: Scher RK, Daniel CR 3 rd , editors. Nails: Diagnosis, therapy, surgery. 3 rd ed, Philadelphia: Elsevier Saunders; 2005. P. 37-70.
[Google Scholar]
|
| 14. |
Tirado-González M, González-Serva A. The nail plate biopsy may pick up gout crystals and other crystals. Am J Dermatopathol 2011;33:351-3.
[Google Scholar]
|
| 15. |
Grover C, Bansal S, Nanda S, Reddy BS, Kumar V. En bloc excision of proximal nail fold for treatment of chronic paronychia. Dermatol Surg 2006;32:393-8; discussion 398-9.
[Google Scholar]
|
| 16. |
Kim JE, Ahn HS, Cheon MS, Lee KJ, Cho BK, Park HJ. Proximal nail fold-lunula double punch technique: A less invasive method for sampling nail matrix without nail avulsion. Indian J Dermatol Venereol Leprol 2011;77:346-8.
[Google Scholar]
|
| 17. |
Zaias N. The longitudinal nail biopsy. J Invest Dermatol 1967;49:406-8.
[Google Scholar]
|
| 18. |
Grover C, Khandpur S, Reddy BS, Chaturvedi KU. Longitudinal nail biopsy: Utility in 20-nail dystrophy. Dermatol Surg 2003;29:1125-9.
[Google Scholar]
|
| 19. |
Fleckman P, Omura EF. Histopathology of the nail. Adv Dermatol 2001;17:385-406.
[Google Scholar]
|
| 20. |
Scher RK, Ackerman AB. Subtle clues to diagnosis from biopsies of nails: The value of nail biopsy for demonstrating fungi not demonstrable by microbiologic techniques. Am J Dermatopathol 1980;2:55-7.
[Google Scholar]
|
| 21. |
Machler BC, Kirsner RS, Elgart GW. Routine histologic examination for the diagnosis of onychomycosis: An evaluation of sensitivity and specificity. Cutis 1998;61:217-9.
[Google Scholar]
|
| 22. |
Tosti A, Bardazzi F, Piraccini BM, Fanti PA. Idiopathic trachyonychia (twenty-nail dystrophy): A pathological study of 23 patients. Br J Dermatol 1994;131:866-72.
[Google Scholar]
|
| 23. |
Tosti A, Fanti PA, Morelli R, Bardazzi F. Trachyonychia associated with alopecia areata: A clinical and pathologic study. J Am Acad Dermatol 1991;25:266-70.
[Google Scholar]
|
| 24. |
Taniguchi S, Kutsuna H, Tani Y, Kawahira K, Hamada T. Twenty-nail dystrophy (trachyonychia) caused by lichen planus in a patient with alopecia universalis and ichthyosis vulgaris. J Am Acad Dermatol 1995;33:903-5.
[Google Scholar]
|
| 25. |
Grover C, Bansal S, Nanda S, Reddy BS. Efficacy of triamcinolone acetonide in various acquired nail dystrophies. J Dermatol 2005;32:963-8.
[Google Scholar]
|
| 26. |
Tosti A, Piraccini BM, Cambiaghi S, Jorizzo M. Nail lichen planus in children: Clinical features, response to treatment, and long-term follow-up. Arch Dermatol 2001;137:1027-32.
[Google Scholar]
|
| 27. |
Peluso AM, Tosti A, Piraccini BM, Cameli N. Lichen planus limited to the nails in childhood: Case report and literature review. Pediatr Dermatol 1993;10:36-9.
[Google Scholar]
|
| 28. |
Tosti A, Peluso AM, Misciali C, Cameli N. Nail lichen striatus: Clinical features and long-term follow-up of five patients. J Am Acad Dermatol 1997;36:908-13.
[Google Scholar]
|
| 29. |
Mann RJ, Allen BR. Nail dystrophy due to sarcoidosis. Br J Dermatol 1981;105:599-601.
[Google Scholar]
|
| 30. |
Sonnex TS, Dawber RP, Zachary CB, Millard PR, Griffiths AD. The nails in adult type 1 pityriasis rubra pilaris: A comparison with Sézary syndrome and psoriasis. J Am Acad Dermatol 1986;15:956-60.
[Google Scholar]
|
| 31. |
Rice RH, Crumrine D, Hohl D, Munro CS, Elias PM. Cross-linked envelopes in nail plate in lamellar ichthyosis. Br J Dermatol 2003;149:1050-4.
[Google Scholar]
|
| 32. |
Cigna E, Palumbo F, De Santo L, Edoardo Zampieri A, Soda G. Short-scar surgical approach for the treatment of glomus tumor of the digit. J Cutan Med Surg 2011;15:21-8.
[Google Scholar]
|
| 33. |
Ma D, Darling T, Moss J, Lee CC. Histologic variants of periungual fibromas in tuberous sclerosis complex. J Am Acad Dermatol 2011;64:442-4.
[Google Scholar]
|
| 34. |
Dalle S, Depape L, Phan A, Balme B, Ronger-Savle S, Thomas L. Squamous cell carcinoma of the nail apparatus: Clinicopathological study of 35 cases. Br J Dermatol 2007;156:871-4.
[Google Scholar]
|
| 35. |
Gallouj S, Harmouch T, Soughi M, Baybay H, Meziane M, Hammas N, et al. Subungual verrucous carcinoma of the toe. Ann Dermatol Venereol 2010;137:842-3.
[Google Scholar]
|
| 36. |
Bolliger A, Gross R. Ammonia, urea and uric acid content of toenails in renal insufficiency and gout. Aust J Exp Biol Med Sci 1953;31:385-90.
[Google Scholar]
|
| 37. |
Piérard GE, Arrese JE, De Doncker P, Piérard-Franchimont C. Present and potential diagnostic techniques in onychomycosis. J Am Acad Dermatol 1996;34:273-7.
[Google Scholar]
|
Fulltext Views
8,481
PDF downloads
2,287





