Translate this page into:
Linear granuloma annulare localized to the finger
2 Department of Dermatology, Tianjin Academy of Traditional Chinese Medicine Affiliated Hospital, Tianjin, China
Correspondence Address:
Litao Zhang
354 Beima Road, Hongqiao District, Tianjin 300120
China
| How to cite this article: Gu A, Liang J, Zhang L, Xiao Y. Linear granuloma annulare localized to the finger. Indian J Dermatol Venereol Leprol 2020;86:314-316 |
Sir,
Granuloma annulare is a noninfectious granulomatous skin disease and presents with a wide variety of clinical manifestations. However, cases of linear pattern, especially with finger involvement, are very rare.[1],[2] Herein, we report an unusual case of this disease with a solitary, linear plaque confined to the lateral aspect of the right index finger without classical lesions elsewhere.
A 23-year-old woman presented with an isolated linear plaque on her right index finger for 10 years. The lesion was preceded by an insect bite which led to a local nonpurulent inflammatory reaction and erythema. Subsequently, a plaque developed at the site and slowly extended in a linear fashion. Cutaneous examination revealed a flesh-colored, linear plaque along the lateral aspect of the right index finger and proximal to the tip of this finger unassociated with any itch or pain. The lesion was a shiny infiltrated plaque of a size of about 8 sq cm with central focal atrophy [Figure - 1]. No similar lesions were found on any other part of the patient's body. Laboratory tests were not remarkable and included a negative human immunodeficiency virus test and negative T-SPOT.TB assay. Furthermore, X-ray examination of the index finger ruled out any osseous involvement.
 |
| Figure 1: A flesh-colored, linear plaque along the lateral aspect of the right index finger and proximal to the tip of this finger |
Histopathology from a skin excision biopsy showed palisading granuloma surrounding a central core of necrobiotic collagen and mucin in the upper dermis [Figure - 2]a. There were a few multinucleated histiocytes and numerous lymphocytes. In addition, dermal mucin deposition was confirmed with Alcian blue staining [Figure - 2]b.
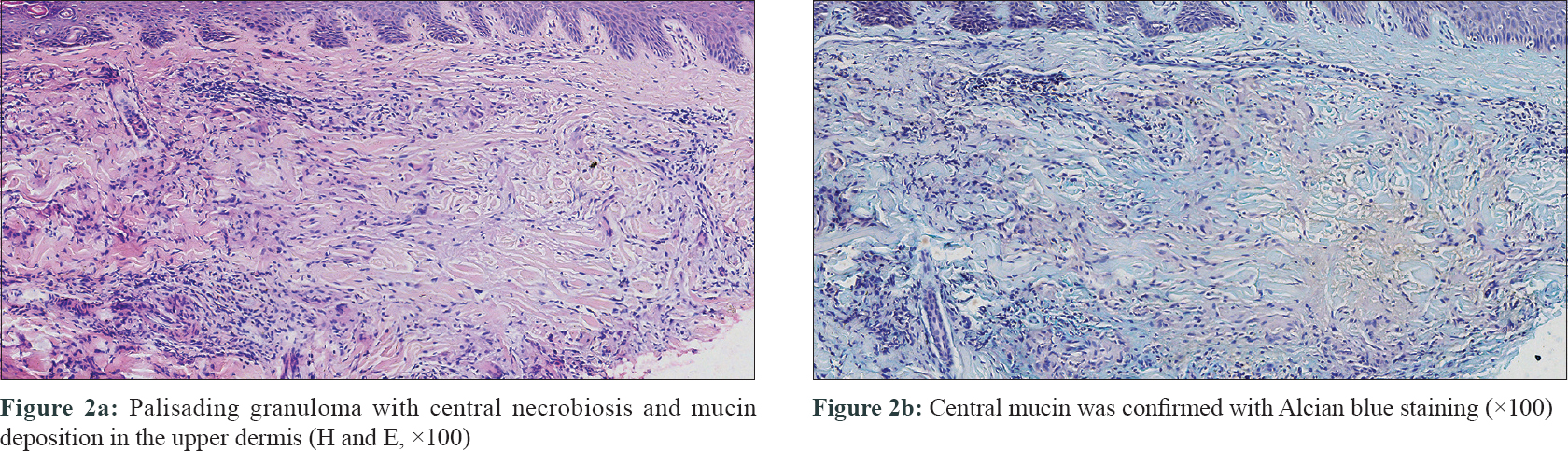 |
| Figure 2: |
The condition was diagnosed as linear granuloma annulare and was treated with betamethasone injection (1 mL), given intralesionally once every 2 weeks for three times, combined with triamcinolone acetonide (0.2%) and neomycin (5000μ/g) paste application once a day for 1 week and repeated every other week for 1.5 months. Follow-up of the patient after 8 months so far revealed satisfactory healing of the lesion with no evidence of recurrence or appearance of any new lesions.
Granuloma annulare is a benign granulomatous disease and can present anywhere on the body. Two-thirds of the patients with this disease are less than 30 years of age and the female-to-male ratio is approximately 2:1.[1] Its primary manifestation is skin-colored or violaceous firm papules in an annular configuration on the upper extremities. In addition to the classical type, other clinical variants include generalized, perforating and subcutaneous as well as three uncommon subtypes: patch, papular and linear or segmental. Despite being a benign disease, it can be associated with more serious conditions such as HIV, solid organ tumors, Hodgkin disease, non-Hodgkin lymphoma and granulomatous mycosis fungoides.[1] In these patients, the clinical manifestation is frequently atypical with painful lesions at unusual locations, including the palms and soles. However, our patient did not suffer any of these mentioned diseases.
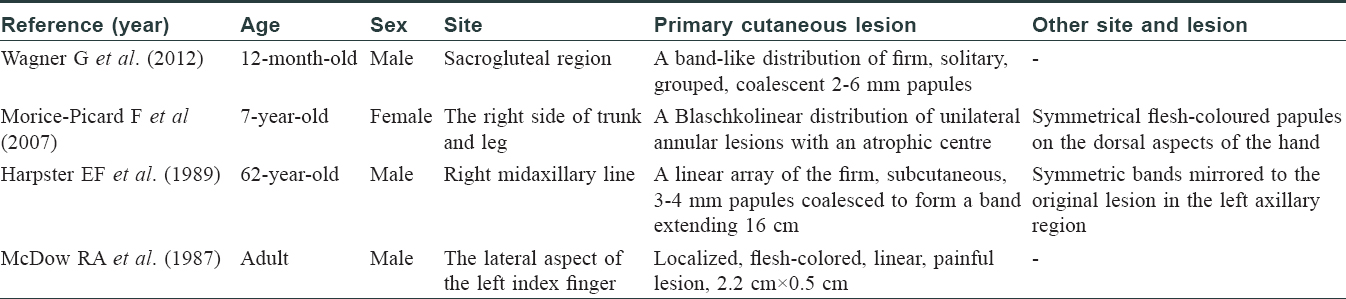
A literature search revealed only four reported linear or Blaschkoid distribution cases [Table - 1].[2],[3],[4],[5] In all these cases, papules or nodules in linear distribution represented the primary lesions with or without classical annular-nodular formation elsewhere. Morice-Picard et al. figured that the Blaschkolinear pattern, which usually corresponds to mostly epidermal defects in monogenic disorders, suggested in their case an autosomal dominant model with a mutation in a gene directly influencing skin homeostasis.[3] Our observations emphasized the hypothesis that stimuli under certain conditions can lead to a linear distribution of common inflammatory dermatosis. Interestingly, our patient developed the skin lesion after an insect bite which might be the trigger to the onset of primary degeneration of the connective tissue at the site of injury.
McDow and Fields in 1987 reported the first case of linear granuloma annulare of the finger.[2] We believe that our case was the second one confined to a similar location. It might be misdiagnosed as other clinical conditions, including discoid lupus erythematosus, sarcoidosis, tuberculosis verrucosa cutis and cutaneous lymphoid hyperplasia which could be ruled out on histopathologic findings and/or laboratory tests.
Granuloma annulare may be a self-limited disease. In our case, the patient suffered from the disease for more than 10 years and showed no sign of spontaneous resolution. Hence, we provided both intralesional as well as topical steroid treatment which were successful in clearing the lesion. Post-treatment follow-up is important because of the tendency of the lesion to recur.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal the identity but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Hu SW, Kaplan J, Patel RR, Kamino H. Trauma-related papular granuloma annulare. Dermatol Online J 2013;19:20719.
[Google Scholar]
|
| 2. |
McDow RA, Fields JP. Linear granuloma annulare of the finger. Cutis 1987;39:43-4.
[Google Scholar]
|
| 3. |
Morice-Picard F, Boralevi F, Lepreux S, Labrèze C, Lacombe D, Taïeb A. Severe linear form of granuloma annulare along Blaschko's lines preceding the onset of a classical form of granuloma annulare in a child. Br J Dermatol 2007;157:1056-8.
[Google Scholar]
|
| 4. |
Harpster EF, Mauro T, Barr RJ. Linear granuloma annulare. J Am Acad Dermatol 1989;21:1138-41.
[Google Scholar]
|
| 5. |
Wagner G, Schmoll J, Sachse MM. Linear granuloma annulare in an infant – An unusual clinical presentation. J Dtsch Dermatol Ges 2012;10:434-5.
[Google Scholar]
|
Fulltext Views
3,859
PDF downloads
1,645





