Translate this page into:
A study of the association of acanthosis nigricans with subclinical atherosclerosis
2 Medical Research Division, UMAE Pediatric Hospital, CMNO, IMSS, Guadalajara, Jalisco, México
3 Cardiotest Laboratory of Echocardiography, Bernardette Hospital, Guadalajara, Jalisco, México
4 Cardiovascular Research Unit, CUCS, University of Guadalajara, Guadalajara, Jalisco, México
Correspondence Address:
Alberto Tlacuilo-Parra
Monte Olimpo 1413, Colonia Independencia, CP 44340, Guadalajara, Jalisco
México
| How to cite this article: Guevara-Guti�rrez E, Tlacuilo-Parra A, Gutiérrez-Fajardo P, Sánchez-Tenorio T, Barba-Gómez F, Miranda-Díaz A. A study of the association of acanthosis nigricans with subclinical atherosclerosis. Indian J Dermatol Venereol Leprol 2017;83:190-194 |
Abstract
Background: Hyperinsulinism is related to the presence of acanthosis nigricans and atherosclerosis; however, we were unable to find any study on the prevalence of atherosclerosis in acanthosis nigricans.Aims: To evaluate the prevalence of carotid atherosclerosis and metabolic alterations in Mexican patients with acanthosis nigricans.
Methods: We carried out a cross-sectional study that included 45 patients with acanthosis nigricans, age- and gender-matched with 45 healthy participants. Volunteers with any comorbidity or taking weight reduction, glucose- and/or lipid-lowering medication or drugs capable of causing acanthosis nigricans were not included in the study. B-mode ultrasound tests were done to measure the carotid intima-media thickness. Body mass index, insulin, glucose and lipid blood serum levels were measured. Chi-square or Fisher's exact test and paired Student t-test were used for statistical analysis.
Results: Carotid intima-media thickness was greater in patients with acanthosis nigricans (mean 0.52 mm vs. 0.46 mm, P = 0.002). The prevalence of abnormal intima-media thickness was higher in patients with acanthosis nigricans versus healthy participants (62.2% vs. 35.5%, P = 0.02). The same occurred with hyperinsulinemia (73.3% vs. 13.3%, P< 0.001), insulin resistance (86.6% vs. 33.3%, P< 0.001), obesity (86.6% vs. 13.3%, P< 0.001) and dyslipidemia (95.5% vs. 77.7%, P = 0.01).
Limitations: The sample size is small and serum markers of cardiovascular risk were not measured.
Conclusion: Acanthosis nigricans is a skin marker for metabolic disturbances and is also associated with carotid atherosclerosis, a finding which is not well documented. We propose that individuals with acanthosis nigricans should be routinely evaluated for these cardiovascular risks.
Introduction
The majority of patients with acanthosis nigricans present with insulin resistance and hyperinsulinemia.[1],[2] Both play a key role in the pathogenesis of atherosclerosis.[3] Despite the fact that some authors mention that acanthosis nigricans must be considered as a skin marker of early atherosclerosis, there are no studies corroborating this relation.[4] Measurement of carotid intima-media thickness with B-mode ultrasound is a useful, precise and noninvasive method for the detection of atherosclerosis in subclinical stages of the illness.[5] An increase in the carotid intima-media thickness is related to the prevalence and extension of coronary artery disease, incidence of cerebral events and generalized atherosclerosis.[6] Our objective was to determine the prevalence of subclinical atherosclerosis and metabolic changes in patients with acanthosis nigricans.
Methods
A cross-sectional study was carried out in a third level dermatological institution. The study was approved by the Local Ethics Committee. Each of the included individuals was explained about the study objectives and procedures and signed informed consent was obtained. The sample size was calculated according to a formula comparing two proportions with a confidence interval of 95%, an α error 5.0% (0.05), a β power of 20% (0.20), therefore the (1−β) power was 80.0% (0.80) with a 1:1 relation between groups. The expected prevalence of hyperinsulinemia in patients with acanthosis nigricans was 50.0% and between healthy individuals 20.0%.[1]
Patients over 18 years of age of either gender, and with a clinical and histopathological diagnosis of acanthosis nigricans were included in the study. Participants were age- (±1.0 year) and gender-matched with clinically healthy subjects. Patients with cutaneous diseases associated with acanthosis nigricans, endocrine illnesses, using medications associated with the development of this condition, weight reduction medications and blood glucose or lipid-lowering drugs and corticosteroids were excluded from the study. Each participant was evaluated as follows:
- A structured questionnaire was administered and included age, gender, family and personal history of diabetes mellitus, hypertension and endocrine diseases, as well as recent intake of any type of drugs. A complete dermatological examination was performed and anthropometric measurements were taken to obtain the body mass index (kg/m [2]).[7]
- A 10 mL venous blood sample (after a 12 h fast) was used for the determination of glucose (≥126.0 mg/dL considered diagnostic for diabetes mellitus),[8] serum lipids:[9] total cholesterol (abnormal >200.0 mg/dL), low-density lipoproteins (abnormal >130.0 mg/dL), high-density lipoproteins (abnormal <40.0 mg/dL), triglycerides (abnormal >150.0 mg/dL), insulin (hyperinsulinemia >17.0 µU/mL)[10] and insulin resistance according to the homeostatic model assessment (glucose [mg/dL] × insulin [μU/mL]/405.0)[11] considering insulin resistance >2.4.[12]
- Carotid ultrasound was done to measure intima-media thickness (measured along a centimeter of the distal wall of the common left and right carotid arteries).[6] All ultrasound measurements were semi-automatic and done by the same (blinded) cardiologist, with Philips iE33 high-resolution B-mode equipment and L11-3 transducer (Philips International B.V., Amsterdam, The Netherlands). Participants were examined lying in the face-up position with their neck extended and the opposite cheek toward the side not being examined. Measurements were obtained at three points and the mean value was calculated to obtain the intima-media thickness of the right and left carotid arteries.[13]
To analyze the results, the SPSS statistical package (v. 15.0, IBM Corporation, Somers, NY, USA) was used. Statistical analysis included central tendency and dispersion measurements. Chi-square test or Fisher's exact test and paired Student's t-test for independent samples (acanthosis nigricans vs. healthy group) were used. The odds ratio was determined (95% confidence interval). Multivariate linear regression analysis was used for the independent predictors of carotid intima-media thickness where the dependent variable was carotid intima-media thickness and the significant predictors in the correlation (body mass index, triglycerides, high-density lipoprotein-cholesterol, insulin and homeostatic model assessment index) were included in the model; P < 0.05 was considered significant.
Results
Forty-five patients with acanthosis nigricans were included in the study; of which 26 (57.7%) were females. The mean age for the acanthosis nigricans group was 38.0 ± 11.1 years (range: 18–61 years) and 37.9 ± 11.0 years for the healthy group (range: 19–60 years, P = 0.97).
Metabolic disturbances
There was a greater prevalence of obese (body mass index ≥30.0) and overweight (body mass index 25.0–29.9) individuals in the study population; hypertriglyceridemia and lower levels of high-density lipoprotein were also greater among patients with acanthosis nigricans. Mean body mass index in patients with acanthosis nigricans was 36.3 ± 6.2 (24.4–53.7) versus 25.1 ± 4.1 (18.5–38.4, P < 0.001). Mean triglyceride level was 213.5 ± 108.2 mg/dL (75.0–474.0 mg/dL) versus 158.7 ± 162.5 mg/dL (32.0–312.0 mg/dL, P = 0.06). Mean high-density lipoprotein level was 32.3 ± 5.9 mg/dL (22.0–49.0 mg/dL) versus 41.4 ± 11.7 mg/dL (23.0–79.0 mg/dL, P < 0.001).
The mean fasting glucose level in patients with acanthosis nigricans was 94.6 ± 19.4 mg/dL (74.0–186.0 mg/dL) versus 82.3 ± 9.1 mg/dL (63.0–106.0 mg/dL, P < 0.001). In the acanthosis nigricans group, three (6.6%) patients were diagnosed with diabetes mellitus versus no cases in the healthy group (P = 0.24). The mean insulin serum level in the acanthosis nigricans group was 24.9 ± 12.5 µU/mL (6.8-64.5 µU/mL) versus 11.4 ± 10.7 µU/mL (3.8–26.8 µU/mL, P < 0.001). The mean homeostatic model assessment index was 6.0 ± 3.8 (1.3–21.8) in the acanthosis nigricans group versus 2.3 ± 2.2 (0.8–15.3, P < 0.001).
Carotid atherosclerosis
In the acanthosis nigricans group, the mean intima-media thickness of the right common carotid artery was 0.51 ± 0.11 mm (0.41–0.99 mm) versus 0.46 ± 0.06 mm (0.40–0.71 mm, P = 0.01). The mean intima-media thickness of the left common carotid artery was 0.54 ± 0.11 mm (0.40–0.94 mm) versus 0.47 ± 0.05 mm (0.40–0.60 mm, P < 0.001). Carotid intima-media thickness was considered abnormal if >0.52 mm (corresponding mean value of the healthy group plus one standard deviation). The prevalence of an abnormal carotid intima-media thickness was greater in patients with acanthosis nigricans, 28 (62.2%) versus 16 (35.5%, P = 0.02) [Figure - 1]. Of the 36 participants with acanthosis nigricans who had a family history of diabetes, 23 (63.8%) had carotid atherosclerosis compared to 7 (33.3%) of the 21 healthy participants without acanthosis nigricans, but with a family history of diabetes (odds ratio = 3, 95% confidence interval: 1–13, P = 0.02). [Table - 1] summarizes the results for the principal variables studied. In patients with acanthosis nigricans, we found a strong positive correlation between carotid intima-media thickness with insulin resistance (r = 0.8, P = 0.001) and hyperinsulinism (r = 0.6, P = 0.006), [Table - 2].
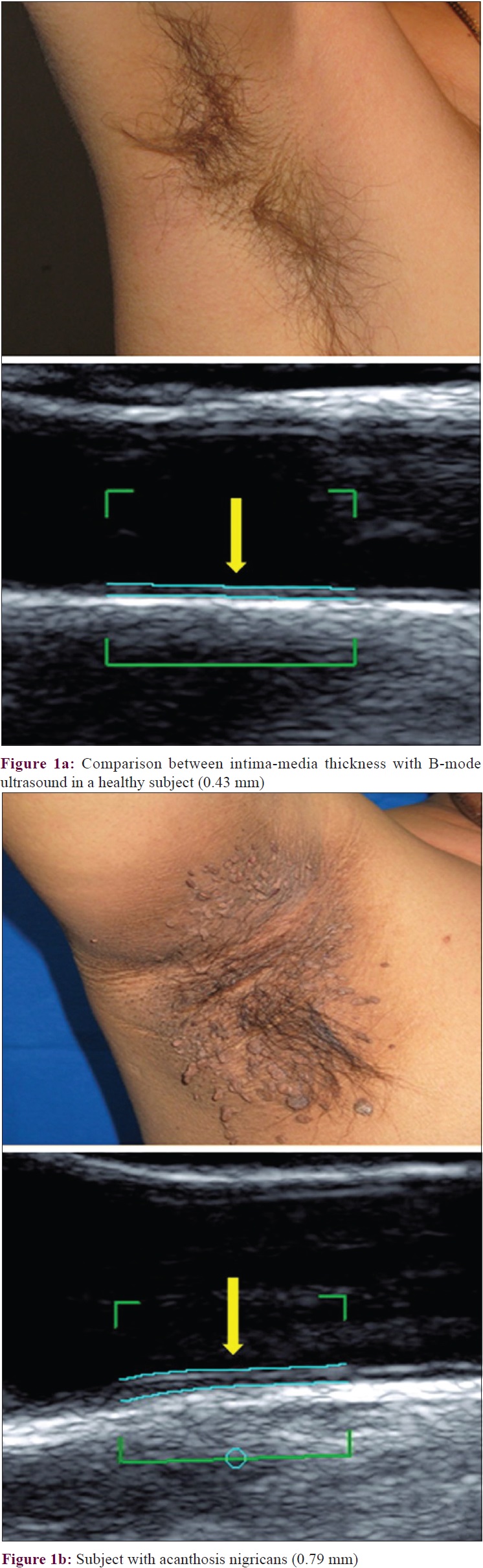 |
| Figure 1 |


Overweight/obesity
Overweight/obese patients were investigated for the presence of hyperinsulinemia and insulin resistance. Both were more prevalent in patients with acanthosis nigricans. The mean carotid intima-media thickness in the acanthosis nigricans group was 0.53 ± 0.11 mm (0.41–0.94 mm) versus 0.49 ± 0.07 mm (0.4–0.71 mm, P = 0.007). [Table - 3] compares the participants with overweight/obesity with and without acanthosis nigricans.

Discussion
Patients with acanthosis nigricans have a prevalence of obesity of 86.6%, indicating 35 times greater risk than the healthy group. A prevalence of 69.0% has been reported by Varthakavi et al. in India [14] while 76.0% prevalence has been found by Araújo et al. in Brazil.[15]
The mean glucose level in acanthosis nigricans patients was greater than in controls, but there was no difference in the prevalence of diabetes mellitus between groups. Araújo et al. reported similar findings.[15] The prevalence of diabetes mellitus in family members was greater in the acanthosis nigricans group, and is a risk factor for its later development in this group of patients; the risk increases with each additional factor such as obesity, which is also more likely to be present in patients with acanthosis nigricans.[16]
The prevalence of hyperinsulinemia in the acanthosis nigricans group with obesity was 75.0% compared to 21.7% in the group with obesity but without acanthosis nigricans. Some authors therefore consider acanthosis nigricans as an independent predictor of hyperinsulinemia.[1] When hyperinsulinemia is present without fasting hyperglycemia, as in 96.9% of our patients, it is considered a risk factor for coronary artery disease.[17]
We also found an association between acanthosis nigricans and insulin resistance. This was independent from obesity, as its prevalence was greater in patients obese or overweight patients with acanthosis nigricans, with five times higher risk for developing insulin resistance than patients who were overweight or obese but without acanthosis nigricans. The greater prevalence of insulin resistance in patients with this condition is highly relevant because it is a primary risk factor for the development of diabetes and dyslipidemia.[18]
The prevalence of hypertriglyceridemia was higher in the group with acanthosis nigricans with a 5-fold greater risk. The explanation for this may be that patients with acanthosis nigricans have insulin resistance, which reduces lipoprotein lipase activity, an enzyme that transforms triglycerides into free fatty acids, resulting in inappropriate lipolysis with a reduction in the capacity to eliminate circulating lipids and elevation of serum triglycerides.[3] The risk for lower levels of high-density lipoprotein in the acanthosis nigricans group was seven times greater. The importance of this result lies in the fact that lower levels of high-density lipoprotein cholesterol are associated with higher cardiovascular risks.[19]
The prevalence of subclinical atherosclerosis was higher in acanthosis nigricans. Insulin resistance was the principal risk factor, although overweight or obese patients are also more likely to develop it. Carotid intima-media thickness was significantly greater in patients with acanthosis nigricans, especially in the overweight/obese group. Therefore, acanthosis nigricans patients have a four fold higher prevalence of subclinical atherosclerosis, as demonstrated by an abnormal carotid intima-media thickness. To the best of our knowledge, this finding has not been described in previous publications. In patients with acanthosis nigricans and a family history of diabetes, the prevalence of carotid atherosclerosis was greater than those with a family history of diabetes, but without acanthosis nigricans, with a three times higher chance of atherosclerosis.
These results cannot be attributed to age and gender because the study groups were paired. Medication use was also not likely to be an influencing factor, because none of the included cases had a previous or actual history of using medications with known cardiac effects. Therefore, we consider that the presence of atherosclerosis is principally attributable to the common pathogenic pathway of hyperinsulinemia/insulin resistance that exists between acanthosis nigricans and atherosclerosis. We could not find other studies for comparison of these findings.
Acanthosis nigricans could be considered a skin marker for subclinical atherosclerosis, and not only for metabolic disturbances as reported previously. Recognition of this condition offers an opportunity to practice preventive medicine, identifying patients with these alterations and offering timely treatment which could reduce cardiovascular risk factors. Due to the current obesity and diabetes pandemic, physicians (and especially dermatologists) should educate patients with acanthosis nigricans about this skin condition and the probable association with metabolic disturbances and/or carotid atherosclerosis.
Some limitations of our study are the small sample size and the lack of serum markers of cardiovascular risk such as the highly sensitive c-reactive protein. This measurement could be correlated with the presence of atherosclerosis to support our findings. Therefore, studies with a larger sample size and adequate patient follow-up should be carried out to search for definitive outcome variables of cardiovascular risk, such as myocardial infarction or revascularization rates in individuals with acanthosis nigricans.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Stoddart ML, Blevins KS, Lee ET, Wang W, Blackett PR; Cherokee Diabetes Study. Association of acanthosis nigricans with hyperinsulinemia compared with other selected risk factors for type 2 diabetes in Cherokee Indians: The Cherokee diabetes study. Diabetes Care 2002;25:1009-14.
[Google Scholar]
|
| 2. |
Torley D, Bellus GA, Munro CS. Genes, growth factors and acanthosis nigricans. Br J Dermatol 2002;147:1096-101.
[Google Scholar]
|
| 3. |
Razani B, Chakravarthy MV, Semenkovich CF. Insulin resistance and atherosclerosis. Endocrinol Metab Clin North Am 2008;37:603-21.
[Google Scholar]
|
| 4. |
Dwivedi S, Jhamb R. Cutaneous markers of coronary artery disease. World J Cardiol 2010;2:262-9.
[Google Scholar]
|
| 5. |
Bots ML, Hofman A, De Jong PT, Grobbee DE. Common carotid intima-media thickness as an indicator of atherosclerosis at other sites of the carotid artery. The Rotterdam study. Ann Epidemiol 1996;6:147-53.
[Google Scholar]
|
| 6. |
Amato M, Montorsi P, Ravani A, Oldani E, Galli S, Ravagnani PM, et al. Carotid intima-media thickness by B-mode ultrasound as surrogate of coronary atherosclerosis: Correlation with quantitative coronary angiography and coronary intravascular ultrasound findings. Eur Heart J 2007;28:2094-101.
[Google Scholar]
|
| 7. |
World Health Organization. Obesity and Overweight, Fact Sheet No. 311. Available from: http://www.who.int/mediacentre/factsheets/fs311/. [Last updated on 2016 Jun 25].
[Google Scholar]
|
| 8. |
American Diabetes Association (ADA). Standards of medical care in diabetes. I. Classification and diagnosis. Diabetes Care 2008;31:S12-3.
[Google Scholar]
|
| 9. |
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002;106:3143-421.
[Google Scholar]
|
| 10. |
Cardona-Muñoz EG, Cardona-Müller D, Totsuka-Sutto S, Nuño-Guzmán CM, Pascoe-González S, Romero-Prado M, et al. Association of hyperinsulinemia with left ventricular hypertrophy and diastolic dysfunction in patients with hypertension. Rev Med Chil 2007;135:1125-31.
[Google Scholar]
|
| 11. |
Bonora E, Targher G, Alberiche M, Bonadonna RC, Saggiani F, Zenere MB, et al. Homeostasis model assessment closely mirrors the glucose clamp technique in the assessment of insulin sensitivity: Studies in subjects with various degrees of glucose tolerance and insulin sensitivity. Diabetes Care 2000;23:57-63.
[Google Scholar]
|
| 12. |
Aguilar-Salinas CA, Olaiz G, Valles V, Torres JM, Gómez Pérez FJ, Rull JA, et al. High prevalence of low HDL cholesterol concentrations and mixed hyperlipidemia in a Mexican nationwide survey. J Lipid Res 2001;42:1298-307.
[Google Scholar]
|
| 13. |
Ebrahim S, Papacosta O, Whincup P, Wannamethee G, Walker M, Nicolaides AN, et al. Carotid plaque, intima media thickness, cardiovascular risk factors, and prevalent cardiovascular disease in men and women: The British Regional Heart study. Stroke 1999;30:841-50.
[Google Scholar]
|
| 14. |
Varthakavi PK, Waingankar A, Patel KL, Wadhwa SL, Khopkar U, Sengupta RA, et al. Acanthosis nigricans: A dermatologic marker of metabolic disease. Indian J Dermatol Venereol Leprol 2002;68:67-72.
[Google Scholar]
|
| 15. |
Araújo LM, Porto MV, Netto EM, Ursich MJ. Association of acanthosis nigricans with race and metabolic disturbances in obese women. Braz J Med Biol Res 2002;35:59-64.
[Google Scholar]
|
| 16. |
Kong AS, Williams RL, Smith M, Sussman AL, Skipper B, Hsi AC, et al. Acanthosis nigricans and diabetes risk factors: Prevalence in young persons seen in Southwestern US primary care practices. Ann Fam Med 2007;5:202-8.
[Google Scholar]
|
| 17. |
Kong AS, Williams RL, Rhyne R, Urias-Sandoval V, Cardinali G, Weller NF, et al. Acanthosis nigricans: High prevalence and association with diabetes in a practice-based research network consortium – A primary care multi-ethnic network (PRIME Net) study. J Am Board Fam Med 2010;23:476-85.
[Google Scholar]
|
| 18. |
Jones LH, Ficca M. Is acanthosis nigricans a reliable indicator for risk of type 2 diabetes? J Sch Nurs 2007;23:247-51.
[Google Scholar]
|
| 19. |
Zureik M, Ducimetière P, Touboul PJ, Courbon D, Bonithon-Kopp C, Berr C, et al. Common carotid intima-media thickness predicts occurrence of carotid atherosclerotic plaques: Longitudinal results from the aging vascular study (EVA) study. Arterioscler Thromb Vasc Biol 2000;20:1622-9.
[Google Scholar]
|
Fulltext Views
3,300
PDF downloads
1,223





