Translate this page into:
Viva questions from the IJDVL
2 Department of Dermatology, K J Somaiya Medical College and Research Centre, Mumbai, Maharashtra, India
Correspondence Address:
Vishalakshi Viswanath
Department of Dermatology, Rajiv Gandhi Medical College, Thane, Maharashtra
India
| How to cite this article: Viswanath V, Vasani R. Viva questions from the IJDVL. Indian J Dermatol Venereol Leprol 2015;81:436-441 |
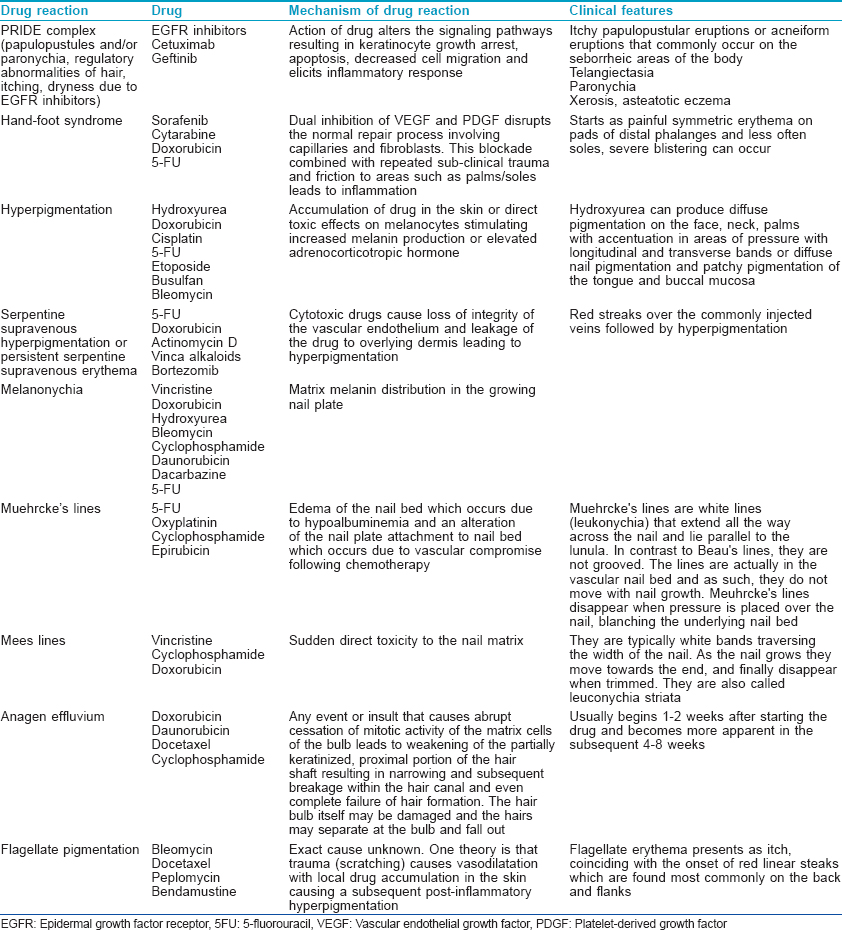
Cutaneous Drug Reactions to Anti-Cancer Drugs
Give a brief outline of the cutaneous drug reactions to anti-cancer drugs
The important cutaneous drug reactions to anti-cancer drugs have been summarized in [Table - 1].
Id Eruption
What is an id reaction?
It is a secondary immunologic reaction to circulating antibodies or activated T lymphocytes that are directed against microbial antigens derived from nonliving organisms.
Enumerate the different types of id reactions?
Different types of id reactions based on their causative factor have been outlined in [Table - 2].

What are the characteristics of a dermatophytid?
- The host harbors the proven focus of infection elsewhere
- Positive skin test response to trichophyton/candida/or epidermophyton
- Fungal forms are neither recoverable from the site of cutaneous eruption nor microscopically visible in direct smears or histopathology preparations
- Lesions resolve spontaneously after an acute course, provided that the infection is identified and eliminated.
What are the clinical presentations of dermatophytids?
- The most common "id" eruption resembles widespread lichen scrofulosorum consisting of bilaterally symmetrical, small, grouped or diffusely scattered, follicular papules usually on the trunk, but may extend on to the extremities in severe cases
- Acutely inflamed tinea pedis may be associated with pompholyx-like vesicles in the web spaces and the sides of the fingers
- Erythema nodosum
- Erythema multiforme
- Erythema annulare centrifugum
- Erysipelas-like id eruption.
Syndromes Discussed in this Issue
Various syndromes have been described in this journal issue. [Table - 3] discusses the salient features of these syndromes.

MACROCHEILIA
Enumerate the differential diagnoses of macrocheilia?
Acute or chronic macrocheilia (enlargement of one or more lips) can be due to various causes as enumerated in Box 1.

What is Miescher′s cheilitis?
Miescher′s cheilitis is another name for granulomatous cheilitis. In this condition, the granulomatous changes are confined to the lip and it is generally regarded as a monosymptomatic form of Melkersson-Rosenthal syndrome (labial edema + scrotal tongue + lower motor neuron type facial palsy), although the possibility remains that these may be two separate diseases. There may be a genetic predisposition and some cases may represent a localized form of sarcoidosis or ectopic Crohn′s disease or orofacial granulomatosis.
The earliest cutaneous manifestations are sudden diffuse or nodular swellings involving the upper lip, lower lip and one or both cheeks, infrequently associated with constitutional symptoms. After the first attack, symptoms usually subside but in subsequent attacks the swelling may persist and slowly increase. It is accompanied by fissured or scrotal tongue in 20-40% of cases and facial palsy in 30% of cases. Facial palsy may be intermittent at first but later becomes permanent. It can be unilateral or bilateral, and partial or complete. Occasionally, other nerves such as auditory, olfactory, glossopharyngeal and hypoglossal are involved.
Treatment options include intralesional steroids, cheiloplasty, clofazimine, metronidazole, erythromycin, sulfasalazine, ketotifen and rarely systemic corticosteroids.
Vitamin D and Skin
Briefly describe the role of topical vitamin D analogs in psoriasis
Various vitamin D analogs, including calcitriol, calcipotriol, tacalcitol, maxacalcitol and hexafluoro-1, 25-dihydroxyvitamin D 3 are useful as topical agents in the treatment of psoriasis. These can be used in combination with agents such as tumor necrosis factor-α inhibitors, methotrexate (MTX), low-dose oral cyclosporine (2 mg/kg/day), oral acitretin, topical dithranol, topical steroids and ultraviolet B therapy.
Thet are useful in chronic plaque psoriasis, scalp psoriasis and nail psoriasis. Vitamin D analogs do not exhibit tachyphylaxis and are effective in the treatment of psoriatic skin lesions in children and in human immunodeficiency virus patients. The use of calcipotriol ointment on face and flexures should be avoided due to its irritancy.
Mechanism
The therapeutic effects of topical vitamin D occur due to the following:
- Vitamin D receptor-mediated genomic mechanism results in inhibition of keratinocyte proliferation
- Non-genomic mechanism induces keratinocyte differentiation by increasing intracellular calcium levels
- Modulation of various markers of epidermal proliferation (proliferating cell nuclear antigen and Ki-67 antigen) and differentiation (involucrin, transglutaminase K, filaggrin, cytokeratins 10, 16) has been shown in situ in lesional psoriatic skin following topical application of vitamin D analogs
- Anti-inflammatory effects of topical vitamin D is due to inhibition of T cell differentiation and proliferation in response to interleukin 1 (IL-1). The anti-inflammatory effects are also due to inhibition of production of IL-2, IL-6 and interferon-gamma. Topical calcipotriol also inhibits human beta defensin 2 (HBD2), HBD3, IL-17A, IL-17F and IL-8 which are found in increased levels in psoriatic lesions, thus it blocks the cathelicidin pathway and reduces inflammation.
Enumerate the role of vitamin D in various dermatological disorders
The role of vitamin D in various dermatological disorders can be grouped into the following categories .
Well established role
Role in etiopathogenesis: psoriasis.
Therapeutic role: psoriasis, lichen sclerosus et atrophicus, morphea.
Inconclusive role
Role in etiopathogenesis: atopic dermatitis, vitiligo, ichthyosis, keloids, autoimmune diseases.
Therapeutic role: skin cancer (prevention), tuberculosis.
Less characterized roles
These include various diseases such as acne vulgaris, rosacea, ageing, seborrheic keratosis, telogen effluvium and female pattern hair loss, leg ulcers, xerosis, Behcet′s disease, autoimmune bullous disorders and polycystic ovarian syndrome with acne and hirsutism.
Pityriasis Rubra Pilaris
Classify pityriasis rubra pilaris
Pityriasis rubra pilaris comprises a group of rare disorders characterized by a cephalo-caudal cutaneous eruption of follicular hyperkeratotic papules with characteristic islands of spared skin along with palmo-plantar keratoderma as a frequent feature.
Griffith′s classification is commonly used and includes:
- Type 1: Classic adult
- Type 2: Atypical adult
- Type 3: Classic juvenile
- Type 4: Circumscribed juvenile
- Type 5: Atypical juvenile.
Pityriasis rubra pilaris associated with immunodeficiency such as human immunodeficiency virus has been added and described as type 6 or human immunodeficiency virus-associated follicular syndrome.
What are the characteristic histological findings in pityriasis rubra pilaris?
The characteristic histological findings are alternating orthokeratosis and parakeratosis (checkerboard pattern), follicular plugging along with dilatation of dermal capillaries and a lympho-histiocytic infiltrate. The foci of parakeratosis are typically seen as areas of perifollicular shouldering (shoulder parakeratosis).
Enumerate treatment modalities for pityriasis rubra pilaris
Supportive treatment with emollients is needed. Retinoids are considered as first line of treatment. Systemic retinoids such as acitretin and isotretinoin can be used in extensive and erythrodermic cases, topical vitamin D analogs are also useful. Other systemic therapies include methotrexate, cyclosporine, phototherapy and biologicals can be tried in resistant cases.
POROKERATOSIS
Enumerate the different types of porokeratosis
Porokeratosis is a group of hereditary or acquired disorders of epidermal keratinization characterized by keratotic lesions with an atrophic center and a prominent peripheral ridge, the histological hallmark of which is the cornoid lamella.
Clinically, seven variants have been identified:
- Plaque type
- Disseminated superficial porokeratosis
- Disseminated superficial actinic porokeratosis
- Linear porokeratosis
- Giant porokeratosis
- Porokeratosis palmaris et plantaris disseminata
- Punctate porokeratosis.
Describe the histological features of porokeratosis
The characteristic histopathological feature is the cornoid lamella seen at the edge of the lesion as a column of poorly staining parakeratotic stratum corneum cells. The granular layer is absent below and the underlying keratinocytes are edematous with spongiosis and shrunken nuclei. A moderate dermal lymphocytic infiltrate may be seen under the lamella. The central area is usually atrophic but may show hyperkeratosis. Uncommonly, a lichenoid pattern and the presence of amyloid material may be detected.
Enumerate treatment modalities in porokeratosis
Topical retinoids, tacalcitol, 5-fluorouracil ointment, imiquimod and systemic retinoids have been tried. Other modalities include cryotherapy, CO 2 laser, pulsed dye laser therapy and photodynamic therapy.
ONYCHOMYCOSIS
What are the clinical patterns of onychomycosis?
Onychomycosis has been classified into five clinical presentations according to the modes of invasion:
- Distal and lateral subungual onychomycosis
- Proximal subungual onychomycosis
- Superficial white onychomycosis
- Endonyx onychomycosis (EO) and
- Mixed onychomycosis (total nail dystrophy, secondary onychomycosis and paronychia -associated onychomycosis).
What is endonyx onychomycosis?
Endonyx onychomycosis is an unusual variant of onychomycosis which involves the inner surface of nail plate without inflammation of the nail bed, onycholysis or subungual hyperkeratosis. The classic nail lesion shows milky-white discoloration in the nail plate without nail surface change. It is caused by Trichophyton soudanense and Trichophyton violaceum.
Bacillary Angiomatosis
What is the etiologic agent in bacillary angiomatosis?
Bacillary angiomatosis is an uncommon infectious vasoproliferative disorder, caused by Bartonella henselae or Bartonella quintana and is commonly associated with immunosuppression. Skin is the most common site of infection. The disease may be preceded by a history of traumatic cat contact or exposure to cat fleas. Ticks, lice and sandflies have also been implicated in the transmission of various Bartonella species.
What are the clinical manifestations of bacillary angiomatosis?
Clinically bacillary angiomatosis has three distinct morphological presentations:
- Pyogenic granuloma-like
- Subcutaneous nodules
- Hyperpigmented indurated plaques
The first type is more common and is characterized by solitary or multiple, reddish, angiomatous papules and nodules affecting different areas of the skin. The face, neck, trunk, extremities and back are most commonly affected. Atypical lesions have been described including those resembling Kaposi′s sarcoma, verruga peruana or leg ulcers. Regional lymphadenopathy can occur and it is often painful. Disseminated disease involves the liver, spleen, lymph nodes, gastrointestinal tract, bone, brain and other organs and can occur without cutaneous lesions.
How is bacillary angiomatosis diagnosed and treated?
Histological examination reveals lobular proliferations of small blood vessels with a diffuse and a predominantly perivascular inflammatory infiltrate involving the superficial and deep dermis. The diagnosis can be confirmed by the demonstration of bacilli in histological sections stained with silver dyes or Warthin-Starry stain. Culture from the biopsied tissues (which can be difficult due to the fastidious nature of organism), electron microscopy examination, serology (which may be unreliable in immunocompromised patients due to lack of antibody response) and polymerase chain reaction are other procedures that can be used to establish the diagnosis.
Long courses of treatment with doxycycline or erythromycin for a period of 8 weeks or longer is recommended.
Fulltext Views
6,048
PDF downloads
2,429





