Translate this page into:
Lichen planus pigmentosus inversus
2 Department of Anatomopathology, Habib Thameur Hospital, Tunis, Tunisia
Correspondence Address:
Houda Hammami Ghorbel
Department of Dermatology, Habib Thameur Hospital, Ali Ben Ayed Street, 1008 Montfleury, Tunis
Tunisia
| How to cite this article: Ghorbel HH, Badri T, Brahim EB, Fenniche S, Benmously R, Mokhtar I. Lichen planus pigmentosus inversus . Indian J Dermatol Venereol Leprol 2014;80:580 |
Sir,
Lichen planus is a common inflammatory dermatosis of unknown origin that presents in a variety of morphologic patterns. Lichen planus pigmentosus inversus (LPPI) is one of the rarer clinical forms. We report six cases of LPPI from North Africa [Table - 1].

Case 1
A 74-year-old woman presented with a 2-week history of brown macules of the neck [Figure - 1]a, axillae, inter- and submammary folds, and groin. Medical history included hypertension treated for many years by captopril, furosemide, and nifedepine. A 1-month application of clobetasol propionate produced no significant response.
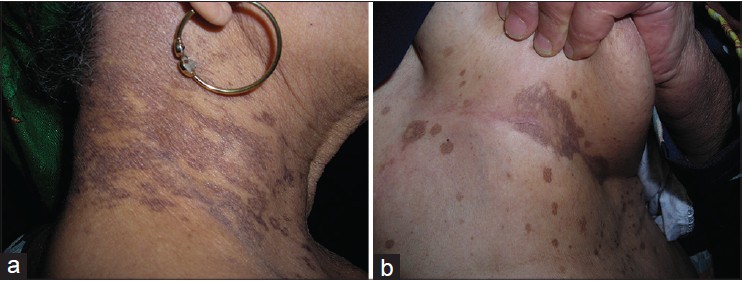 |
| Figure 1: (a) Lichen planus pigmentosus inversus: Pigmented brownish-grey, well-defined macules and plaques located on the neck. (b) Brown, well-demarcated macules and plaques in the submammary folds |
Case 2
A 60-year-old woman, presented with pruriginous and pigmented patches located in the neck, inframammary folds [Figure - 1]b, and presacral area which developed over the last 3 years. The patient received oral prednisone (0.5 mg/kg/day) for 2 months but no improvement was noted.
Case 3
A 54-year-old woman presented with a 2-week history of pruriginous purple-brown macules and plaques in the sub-mammary folds, groin, and genitalia. She received topical betamethasone for several months with no improvement.
Case 4
A 60-year-old woman with a history of diabetes, consulted for pruritic, scaly, violaceous-brown macules, and annular brownish plaques arising in the submammary folds and groin. The patient received topical betamethasone with slight improvement.
Case 5
A 49-year-old woman presented with a 2-week history of pruriginous brownish plaques located symmetrically in the axillae, groin, and vulva. No improvement was obtained with topical betamethasone.
Case 6
A 76-year-old woman presented with a 3-month history of pruriginous, brownish macules and plaques in the sub-mammary folds. The patient was treated with topical betamethasone for 2 months with no improvement.
In all these cases, histological examination revealed atrophic epidermis with hypergranulosis, band-like lymphocytic infiltrate of the upper dermis with abundant colloid bodies, and marked pigmentary incontinence [Figure - 2]. Hyperkeratosis was noted in four cases. Clinical and histological features were consistent with the diagnosis of lichen planus pigmentosus inversus in all patients.
 |
| Figure 2: Thinning of the epidermis, a band-like lymphocytic infiltrate with basal vacuolar change, necrosis of keratinocytes and prominent melanin incontinence in the upper dermis (hematoxylin and eosin, ×40) |
Lichen planus pigmentosus inversus is a rare variant of lichen planus, described by Pock et al. [1] We found previous reports of 21 cases of whom 13 were females and eight males. [1],[2],[3],[4],[5] In our series, all patients were women. The mean duration of symptoms before the diagnosis ranges from 2 months to 15 years. [2] It has been postulated that this condition occurs mainly in Caucasians from central Europe. [1] However, Kashima et al., have described two Japanese patients with the disease. [3] We found only one report of lichen planus pigmentosus inversus in a phototype IV woman [4] and did not find previous reports of the disease in North African dark-skinned persons like our patients. Clinically, the condition is characterized by well-circumscribed violaceous-brown macules confined to intertriginous areas [1] It affects mainly the axillae and groin. [2] In our patients, the submammary folds and groin were the most common sites. Skin lesions of classic lichen planus have been described in non-intertriginous areas in 10% of patients [1] but we did not find them in our patients. Histopathological features are similar to lichen planus but there is a marked pigmentary incontinence in the upper dermis.
The differential diagnosis includes fixed drug eruption, acanthosis nigricans, candida intertrigo, erythrasma, post-inflammatory pigmentation, lichenoid toxic dermatitis or ashy dermatosis. The etiopathogenesis of the condition remains unknown. Captopril is known to induce lichenoid eruptions and the onset of symptoms 1 year after initiation of captopril in our first patient may indicate an association. External stimuli, such as friction (Koebner phenomenon), may be a triggering factor. [5]
Pigmented plaques tend to persist for months. Some authors suggest that treatment with medium or high potency topical corticosteroids or calcineurin inhibitors could accelerate the healing process. In our retrospective study, different treatment regimens of topical and systemic corticosteroids had been used without success.
Lichen planus pigmentosus inversus should be considered in the differential diagnosis of cutaneous pigmentation exclusively located in flexural areas.
| 1. |
Pock L, Jelínková L, Drlík L, Abrhámová S, Vojtechovská S, Sezemská D, et al. Lichen planus pigmentosus-inversus. J Eur Acad Dermatol Venereol 2001;15:452-4.
[Google Scholar]
|
| 2. |
Bennàssar A, Mas A, Julià M, Iranzo P, Ferrando J. Annular plaques in the skin folds: 4 cases of lichen planus pigmentosus-inversus. Actas Dermosifiliogr 2009;100:602-5.
[Google Scholar]
|
| 3. |
Kashima A, Tajiri A, Yamashita A, Asada Y, Setoyama M. Two Japanese cases of lichen planus pigmentosus-inversus. Int J Dermatol 2007;46:740-2.
[Google Scholar]
|
| 4. |
Kim BS, Aum JA, Kim HS, Kim SJ, Kim MB, Oh CK, et al. Coexistence of classic lichen planus and lichen planus pigmentosus-inversus: Resistant to both tacrolimus and clobetasol propionate ointments. J Eur Acad Dermatol Venereol 2008;22:106-7.
[Google Scholar]
|
| 5. |
Ohshima N, Shirai A, Saito I, Asahina A. Lichen planus pigmentosus-inversus occurring extensively in multiple intertriginous areas. J Dermatol 2012;39:412-4.
[Google Scholar]
|
Fulltext Views
4,282
PDF downloads
851





