Translate this page into:
Blepharoplasty and periorbital surgical rejuvenation
Correspondence Address:
Milind Naik
Consultant & Head, Department of Ophthalmic and Facial Plastic Surgery, LV Prasad Eye Institute, Road 2, Banjara Hills, Hyderabad - 500 034
India
| How to cite this article: Naik M. Blepharoplasty and periorbital surgical rejuvenation. Indian J Dermatol Venereol Leprol 2013;79:41-51 |
Abstract
The periorbital region forms the epicenter of facial aging changes and receives highest attention from physicians and patients. The concern about visual function, clubbed with the need for hidden incisions, makes the periocular region a highly specialized surgical area, most appropriately handled by an ophthalmic plastic surgeon. The article provides an overview of cosmetic eyelid and facial surgery in the periocular region. Common aesthetic surgical procedures as well as ocular side-effects of commonly performed periocular injections are discussed from the dermatologist's point of view.Introduction
Ophthalmic plastic surgery primarily deals with disorders of the eyelid, lacrimal apparatus, orbit and periocular cosmetic surgery. Cosmetic surgery is the most rapidly changing sub-discipline of ophthalmic plastic surgery. The ophthalmologist most precisely brings the traditions of precision and finesse that characterize ocular microsurgery to the field of cosmetic facial surgery. This article should serve as an overview of common periocular and facial aesthetic procedures. For the purpose of description, they are divided into upper and mid-face, which represents the periocular region. The first section provides a brief outline of anatomy that is relevant to periocular rejuvenation.
Anatomy of the periorbital region
A detailed understanding of periorbital anatomy is absolutely essential for safe and successful periocular rejuvenation. A brief description of periorbital anatomy from the aging perspective is described here with the help of [Figure - 1].
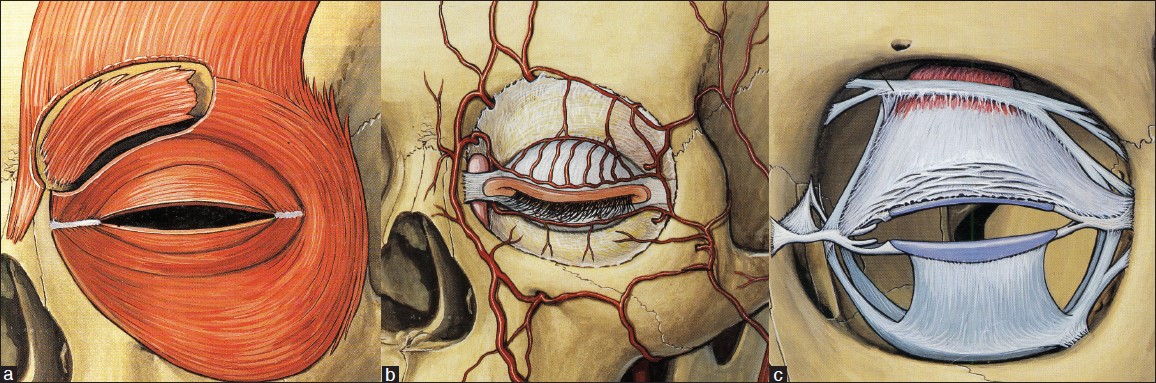 |
| Figure 1: Orbicularis oculi muscle (a), showing the pre-tarsal, pre-septal, and orbital components. Corrugator super-cilii is deep to the orbicularis. Orbital septum (b) extends from bony orbital rim to the eyelid margin and helps contain the orbital fat within the orbit. Behind the septum, the image shows levator muscle in close proximity to superior orbital rim as it attaches to the upper eyelid tarsus (c). Reprinted with permission Atlas of Clinical and Surgical Orbital Anatomy, 1994, Dutton JJ ed. |
The skin covering the orbital opening (mostly composed of eyelid skin) is the thinnest in the body, with minimal or no subcutaneous fat. Immediately underlying it is the orbicularis oculi muscle. It is divided into pre-tarsal, pre-septal, and orbital components as shown in [Figure - 1]a. The orbital part of orbicularis interdigitates with frontalis muscle superiorly and procerus muscle supero-medially. Deeper to the orbital part of orbicularis, along the superior orbital rim, lies the corrugator supercilii muscle. Orbital part of orbicularis and corrugator muscle are brow depressors. The pre-tarsal part of orbicularis in the lower eyelid causes a prominent orbicularis roll. Orbicularis muscle is the only active force that keeps lower eyelid margin in its normal position. Skin approach blepharoplasty can damage this muscle to some extent, thereby posing a risk of lower eyelid retraction. Frontalis muscle is the only brow elevator. Deeper to the orbicularis, lies the orbital septum, which is a thin fibrous connective tissue layer extending from the orbital rim to the eyelid margin [Figure - 1]b. For the sake of understanding, periorbital tissues can be divided into two components, by the orbital septum. Pre-septal tissues include skin, orbicularis, and the superficial vasculature. Post-septal tissues include the eyeball, extraocular muscles, neurovascular structures, and orbital fat. All the post-septal soft tissue lie within the orbit, a conical-shaped bony structure.
Orbital fat remains fairly constant throughout life and does not change with body weight unlike fat from anterior abdominal wall. The orbital septum keeps the orbital fat secure within the orbit. With age, laxity of septum combined with descent of malar fat unmasks the orbital fat, which prolapses out, creating eyelid bags. In the upper eyelid, orbital fat prolapses as two distinct compartments, the central and medial fat pads separated by the superior oblique muscle tendon. The lower eyelid orbital fat is divided into three compartments by the inferior oblique tendon medially and the arcuate expansion laterally into medial, central, and the lateral fat pads.
When the orbital septum is removed, one can notice the levator palpebrae superioris muscle arising from the orbital apex and inserting into the upper eyelid tarsal plate [Figure - 1]c. Its muscular component lies very close to the superior orbital rim, which changes into an aponeurosis as one approaches the lashes. Deep injections of botulinum toxin into corrugator, therefore, have higher chances of seeping into levator muscle to cause ptosis.
Upper face
The upper face lies between the trichion superiorly and the canthi inferiorly. It includes the forehead, eyebrows, upper eyelid, and the mimetic muscles of the forehead and the eyebrows. Commonest aesthetic procedures for the upper face include upper eyelid blepharoplasty, brow-lift surgery, brow volume augmentation, and cosmetic correction of blepharoptosis.
Upper eyelid blepharoplasty
The eyes are an important component of facial aesthetics, and blepharoplasty has a vital positive effect on facial harmony and the perception of aging. Blepharoplasty is one of the most commonly performed facial cosmetic procedures. Symptoms such as tired-looking eyes, excess skin, droopy eyelids, or circles around the eyes may benefit from blepharoplasty. [1] Other facial and skin rejuvenation procedures such as brow or mid-face lift, lasers, or chemical skin resurfacing can often be performed at the same time. [2]
Indications
Upper eyelid blepharoplasty is most commonly performed for ′dermatochalasis,′ which represents excessive, overhanging inelastic upper eyelid skin due to aging [Figure - 2]a-d. Blepharochalasis represents excessive papery thin skin in the upper eyelid in young patients and can also benefit by blepharoplasty [Figure - 2]b. Less frequently, a ′blepharoplasty-like′ excision is required for extensive xanthelasma [Figure - 2]d.
 |
| Figure 2: Typical indications for blepharoplasty include overhanging excessive aging skin in the aged, termed Dermatochalasis (a) and excessive papery-thin skin in young patients, called Blepharochalasis (b). Loss of brow fat volume can give a pseudo-dermatochalasis appearance (c), which needs brow volume augmentation rather than blepharoplasty. Rarely, a blepharoplasty-like incision may be needed for extensive Xanthelasma (d) |
Pre-operative evaluation
Pre-operative patient evaluation for blepharoplasty should document medical and ocular evaluation. In addition to a complete eye examination, the evaluation of the periorbital area should take into account skin quality and quantity, underlying 3-dimentional soft-tissue contours, and the bony skeletal support. Ophthalmologic history should be obtained, including vision, corrective lenses, allergic reactions, excess tearing, and dry eyes.
Surgical principle
A simple upper or lower eyelid blepharoplasty where only skin or fat is excised can be performed under local anesthesia. When more invasive procedures are combined with blepharoplasty, general anesthesia may be required.
Upper eyelid blepharoplasty is almost always performed via anterior approach (skin excision). The aim of surgery is to excise the excess skin between eyelashes and eyebrow, to allow a uniform eyelid fold and clear visual axis, without compromising closure of the eyelids [Figure - 3]. Additional steps include fat sculpting, re-contouring brow fat pad, and a trans-bleph browpexy if that is planned. The lower limit of excision is along the eyelid crease, which is situated 7-9 mm above the lash line, and the horizontal limits are the lateral and medial canthi [Figure - 4]. Minimum 20 mm of vertical lid height should be preserved for normal eye closure [Figure - 4]. Blepharoplasty may be combined with brow-lift, or may involve excision of retro-orbicularis oculi fat (ROOF) to achieve the desired effect [Figure - 5].
 |
| Figure 3: Upper eyelid blepharoplasty for dermatochalasis. Pre-operative appearance (a); Day-1 post-operative, with upper eyelid edema (b); 3 months post-operative appearance showing symmetrical eyelid crease, and a barely visible scar hidden in the eyelid fold (c and d). The brow fat pad still shows minimal deflation, which can later receive volume augmentation |
 |
| Figure 4: Upper eyelid blepharoplasty. Skin marking and measurement is performed to leave minimum 20 mm vertial lid height (a). Subcutaneous injection of local anesthetic agent (b). Skin incision with radiofrequency fine monopolar empire tip (c). Conservative fat sculpting prior to skin closure (d). Reprinted with permission from Naik MN, Honavar SG, Das S, Desai S, Dhepe N. Blepharoplasty: an overview. J Cutan Aesthet Surg 2009;2:6-11 |
 |
| Figure 5: Pre and post-operative photographs following upper eyelid blepharoplasty combined with external brow-lift (a and b) and upper eyelid blepharoplasty combined with retro-orbicularis oculi fat (ROOF) excision (c and d). Reprinted with permission from Naik MN, Honavar SG, Das S, Desai S, Dhepe N. Blepharoplasty: an overview. J Cutan Aesthet Surg 2009;2:6-11 |
Complications
Possible complications include upper eyelid retraction with scleral show from anterior lamellar inadequacy, lagophthalmos, acquired diplopia, and corneal exposure. The most common complication of cosmetic surgery is failure to meet the patient′s expectations.
Eyebrows: Volume Augmentation and Browlift
In periocular aesthetic evaluation, the eyebrow receives special attention as it is a functionally intergral part of upper eyelid complex. Two classical aging changes noted in the eyebrow include deflation (volume loss) and descent (brow ptosis).
Assessment of the Eyebrow
Deflation, or loss of volume, is indicated by loss of the round contour of eyebrow fat pad, leading to skin hooding. It can be best appreciated by comparing the findings with the individual′s old photographs. Brow ptosis should be assessed by evaluating the position of the hair-bearing eyebrow in relation to the superior orbital rim. Normally, it is placed at or above the superior orbital rim. Brow deflation as well as brow ptosis leads to an appearance of ′excess′ upper eyelid skin (pseudo-dermatochalasis). Eyebrow asymmetry is commonly noted as a part of facial asymmetry but can also be an indicator of subtle eyelid ptosis on the side with a higher brow. Brow deflation requires filling (Filler or fat), whereas brow ptosis is corrected by a brow-lift procedure.
Brow volume augmentation
Indications
Brow volume augmentation is indicated when the brow height is normal, but its convex contour is lost due to fat loss.
Injection principle
Brow volume can be augmented by hyaluronic acid fillers or autologous fat transfers. [3] The technique involves injection into the deep sub-brow fat pocket, just above the periosteum. It achieves a fuller brow, eliminates the appearance of ′pseudo-dermatochalasis,′ (which can be erroneously advised a blepharoplasty), and to some extent, also elevates the eyebrow [Figure - 6]. In practice, it is prudent to perform hyaluronic acid filler first and then graduate to a fat transfer after the patient is convinced about the appearance. Brow volume augmentation with autologous fat is commonly performed as an adjunct to blepharoplasty, by direct injection through blepharoplasty incision.
 |
| Figure 6: Brow volume augmentation (a and b) with Hyaluronic acid filler. Note the loss of brow volume (top left), which, when adequately filled, eliminates the overhanging skin and gives a fuller eyebrow with convex contours (b). A tear trough filler was also performed, along with chemodenervation of the forehead to reshape the eyebrow. Orbital rim hollow (tear trough deformity) is another common indication for periorbital filling with hyaluronic acid or autologous fat (c and d) |
Complications
Brow volume augmentation can lead to complications like temporary edema and bruising, irregular filling, and superficial injection. The gravest complication of periocular filler injection is partial or complete blindness (discussed later).
Browlift
Indication
Brow-lift is indicated for aesthetically or functionally significant brow ptosis (eyebrow level below the superior orbital rim).
Surgical principle
The aim of surgery is to place the eyebrow at a higher anatomic location in relation to the orbital rim and to address glabellar frown lines by weakening the corrugator and procerus muscles. Browlift can be performed by several techniques. These include direct browlift (skin excision above the brow) as an adjunct to blepharoplasty (internal browpexy), pre-trichial browlift (incision along the anterior hairline), coronal brow-lift (incision within the scalp in coronal plane), and the minimally invasive, endoscopic approach [Figure - 7]. [4]
 |
| Figure 7: Techniques of surgical brow-lift. External brow-lift (surgeon's view) showing excision of forehead skin above the temporal half of the eyebrow (a); Endoscopic brow-lift showing the forehead dissection through a stab incision in the scalp (b); endoscopic view of the supraorbital periosteum that is released (c), calvarial fixation with titanium screws within the para-sagittal scalp incisions (d), and finally fixation of the entire forehead-brow complex at a higher position on the skull using staples (e) |
The endoscopic approach to forehead lift has become a popular method due to improved aesthetics, minimal scarring, decreased healing time, and greater patient satisfaction. It is best suited for brows with mild to moderate ptosis of up to 1.5 cm. [4]
Surgical technique
Endoscopic brow-lift is performed through hidden sub-centimeter temporal and paramedian incisions within the scalp following local anesthesia with tumescent solution. The entire forehead soft-tissue complex is then dissected off the skull in a sub-periosteal plane, and its periosteal attachments are lysed to allow lifting the eyebrow. The corrugator and procerus muscles can be lysed or sharply dissected. The freed forehead complex is then fixated at a higher position on the bony skull using titanium screws [Figure - 7].
Complications
In addition to bruising and edema, complications include localized alopecia at the incision site and rarely damage to the frontal branch of facial nerve due to faulty technique.
Ptosis surgery
Blepharoptosis means drooping of the upper eyelid. It can be either congenital or acquired. Both pose a cosmetic blemish to the patient, and acquired aponeurotic ptosis is often a common ageing change, leading to sleepy or droopy eyes.
Indications
Adult ptosis surgery is indicated for cosmetic reasons in patients with cosmetically significant asymmetry in eyelid fissure height. It also adds to the functional value by improving the superior field of vision.
Ptosis results from sub-optimal functioning of the levator palpebrae superioris muscle. The cause of ptosis can be diagnosed by an accurate history, duration, progress, and clinical evaluation. Assessment of ptosis includes measurement of the palpebral fissure height (vertical height between the midpoint of upper and lower eyelid in primary gaze) and the levator function.
Surgical principle
Mild ptosis can be corrected by Mullerectomy surgery [Figure - 8] that tightens the posterior eyelid lamina (conjunctiva and Mullers muscle) to predictably raise the eyelid. Mullerectomy totally avoids any skin scar. Moderate ptosis requires anterior approach levator resection surgery [Figure - 8] performed through an eyelid-crease incision. Severe ptosis requires a sling surgery where the ptotic eyelid is connected to the frontalis muscle, thereby lifting the eyelid.
 |
| Figure 8: Mild upper eyelid ptosis (aponeurotic) corrected by Mullerectomy surgery that leaves no cutaneous scar (a and b); Moderate congenital ptosis corrected by anterior approach levator resection surgery where the scar is hidden inside the eyelid fold (c and d) |
Complications
Complications of ptosis correction include ecchymosis, under/over correction and corneal epithelial keratopathy due to lagophthalmos.
The mid-face
The mid-face lies between the lateral canthal angle and the top of the nasolabial fold. It includes the medial and lateral canthal tendon, lower eyelids, sub-orbicularis oculi fat (SOOF), malar fat pad, orbitomalar ligament, orbital septum, and origins of the zygomaticus major and minor muscles and levator labii superioris.
Volumetric distribution of the mid-face soft tissues is an important factor in the youthful appearance of the human face. If these tissues are full relative to the lower face, the individual appears healthy and young. [5]
Commonest aesthetic procedures in the mid-face include lower eyelid blepharoplasty, lower lid fat repositioning, mid-face lift, and volume augmentation of lower eyelid hollows (Fillers/fat).
Assessment of the lower eyelid and mid-face region
Lower eyelids should be assessed for skin excess and fat herniation. Fat bags should be differentiated from fluid festoons since the management is entirely different. Fat prolapse is typically compartmentalized (medial, central, and lateral), is limited inferiorly by the orbital rim, and becomes more prominent in upgaze [Figure - 9]. Fluid festoons on the other hand are primarily within the skin, not restricted by the orbital margin, and are not compartmentalized. Downward displacement of the lateral canthus is an aging change. Orbital rim hollow (tear trough deformity) is also an aging sign, though it can be seen in young adults too [Figure - 9]. Aging can lead to a number of aesthetic changes in the lower eyelid including laxity of the skin, orbicularis or orbital septum, orbital fat prolapse (eyelid bags), canthal laxity, malar festoons, and periocular wrinkles and pigmentation. [4] Lower eyelid rejuvenation is more complex and has several treatment options such as fillers, blepharoplasty, and skin resurfacing. Most cosmetic surgeons today have developed a customized approach to eyelid surgery, in which the specific anatomic problems are identified and the operation is individualized to address these problems.
 |
| Figure 9: Typical aging changes in the lower eyelid and mid-face region. Lower eyelid fat prolapse (fat bags) is compartmentalized into lateral, central, and medial (a); Fluid festoons look similar to fat bags, but need to be differentiated (b); Lower eyelid tear trough (orbital rim hollow) can also appear in young patients (c); A double-bubble appearance (d) needs a fat repositioning procedure |
Lower eyelid blepharoplasty
Lower eyelid blepharoplasty primarily addresses the lower eyelid fat bags, excess lower eyelid skin, and canthal position.
Indications
The transconjunctival approach [Figure - 10] is indicated in most cases with retained skin elasticity because it leaves no external scar and reduces the chance of eyelid retraction and postoperative ectropion than other methods. [6],[7] The transcutaneous approach is preferred only if there is excess skin that requires excision. [8] However, with the newer skin-tightening modalities available to the dermatologist, the transconjuctival approach is most popular and has several advantages over skin approach. [9],[10]
 |
| Figure 10: Transconjunctival blepharoplasty (Surgeon's view). Injection of local anesthetic into the inferior conjunctival fornix (a). Forniceal incision to expose orbital fat (b). Conservative fat excision with radiofrequency monopolar tip (c). Assessment of contours on table (d). Reprinted with permission from Naik MN, Honavar SG, Das S, Desai S, Dhepe N. Blepharoplasty: an overview. J Cutan Aesthet Surg 2009;2:6-11 |
Surgical principle
Transconjunctival lower lid blepharoplasty
For transconjunctival lower lid blepharoplasty, the inferior conjunctival fornix is anesthetized, and fat bags are approached through small incisions within the conjunctiva using radiofrequency monopolar cautery or CO 2 laser. Gentle pressure on the eyeball prolapses the fat compartments, and conservative fat removal is achieved. The tarsoconjunctival incision heals by epithelization without any sutures, and excellent aesthetic outcome is achieved in most cases [Figure - 11].
 |
| Figure 11: Pre- and post-operative photographs following transconjunctival lower eyelid blepharoplasty with conservative fat excision. No external scar, no conjunctival sutures, and no scarring of the orbital septum are the advantages of the transconjunctival approach |
A lateral canthoplasty is often performed along with lower eyelid blepharoplasty. This fixes the lateral canthus at a higher position, thereby stretching the lower eyelid skin and reducting the wrinkles. [4],[11],[12] Wrinkles and excess of vertical skin in the lower eyelid can also be dealt with by skin resurfacing techniques, such as chemical peels and CO 2 or by Erbium-YAG laser resurfacing.
Transcutaneous lower eyelid blepharoplasty
Transcutaneous lower lid blepharoplasty is chosen when excess skin needs to be excised, along with the prolapsed fat [Figure - 12]. The ′skin pinch′ technique removes only skin and is ideal for skin laxity alone. [13] Via a subciliary incision, the skin and orbicularis is dissected up to the level of the inferior orbital rim, periorbital fat is excised, and a thin strip of excess skin can also be excised at closure.
 |
| Figure 12: A middle-aged patient with upper eyelid dermatochalasis, left upper eyelid ptosis, excess lower eyelid skin, and lower lid fat bags (a). He underwent a trans-cutaneous blepharoplasty with conservative fat excision and left Mullerectomy for ptosis. Appearance on Day 1 post op (b), 1 week post op (c), and 3 months post op (d) |
complications
Complications of lower eyelid blepharoplasty include ecchymosis and hematoma, inadequate removal of orbital fat. Trans-cutaneous approach in addition can lead to skin scar, lower lid malposition due to orbicularis denervation.
Lower eyelid fat repositioning
In youth, the eyelid-cheek complex has a single smooth convex profile. With advancing age, thinning of septum, and receding bony orbital rim, pseudo-herniation of orbital fat occurs producing a double convex deformity [Figure - 9]d of the lower eyelid. [14] Simple removal of orbital fat in this situation can result in a hollow appearance of the lower eyelid. Preservation of the lower orbital fat is a new concept in facial rejuvenation. [15]
Indication
Fat repositioning is indicated when excessive lower eyelid fat prolapse is accompanied by a deep orbital rim hollow.
Surgical principle
In fat repositioning surgery, instead of excising, the orbital fat is advanced beyond the infraorbital rim underneath the orbicularis muscle with the help of temporary exteriorized sutures. The fat is placed within the sub-periosteal plane, thereby eliminating the orbital rim hollow and provides more youthful rejuvenation of the mid-face. [14],[16],[17] [Figure - 13] a and b
 |
| Figure 13: Trans-conjunctival lower eyelid fat repositioning (a and b) that eliminates the double bubble appearance. Trans-conjunctival mid-face lift was performed in addition to face-lift (c and d) that elevates the descended mid-face soft tissue. Residual tear trough may need hyaluronic acid fillers or an autologous fat transfer |
Other methods suggested to correct tear trough deformity include orbital fat removal, fat injections or grafts, and alloplastic cheek implants. In general, trans-conjunctival fat repositioning results in leveling of the tear trough deformity, a smooth contour of the lower eyelid, and high patient satisfaction. [18]
Complications
Fat repositioning, if not performed correctly, can lead to lower eyelid retraction or diplopia.
Mid-face lift
Aesthetically, the goal of mid-face lift is to achieve facial rejuvenation by increasing malar fullness, and to reduce the ′′skeletonized′ appearance of the inferior orbital rim [Figure - 13]c. It also reduces the prominence of the nasolabial and nasojugal (tear trough) folds. [19] Functional indications for mid-face lift include lower eyelid retraction secondary to lower blepharoplasty and cicatricial ectropion. [20]
Surgical principle
For correction of mild mid-face descent, trans-conjunctival dissection is extended along inferior orbital rim sub-periosteally, and the cheek soft tissue is lifted by sutures that lift from the fat pad to the periosteum of the infraorbital rim.
When a more robust mid-face suspension is required, incisions are made at the temporal scalp, inferior conjunctiva, and at alveolar oral mucosa. The mid-face is mobilized by sub-periosteal dissection and is lifted towards the deep temporalis fascia while securing it to the inferior orbital rim. [21]
Complications
Mid-face-lift can be complicated by hematoma, lower eyelid retraction, and persistent conjunctival chemosis. Malar hypoesthesia due to temporary paresis if infra-orbital nerve is also possible.
Orbital decompression for prominent eyes
Prominent eyes (proptosis) can be a cosmetic blemish and is seen in high myopias as a familial trait or as a sequel of thyroid eye disease. Decompression surgery involves removal of excessive fat from behind the eye or widening the bony orbit. This allows the prominent eyes to relax back into the socket, giving a more natural look.
Indications
Orbital decompression is indicated for patients with proptosis due to thyroid eye disease, large eyes due to myopia.
Surgical principle
Minimally invasive orbital decompression surgery is performed through incisions hidden within the upper eyelid crease, inferior conjunctival fornix, or trans-caruncular approach [Figure - 14]. [22] Typically, decompression begins with orbital fat removal, and removal of bony wall is added if required as the deep lateral wall, medial wall, and foor in that order to achieve good aesthetic results [Figure - 15].
 |
| Figure 14: Minimally invasive techniques of orbital decompression target the ethmoidal air cells medially (a) via trans-caruncular incision (b). The lateral orbital wall is approached through an eyelid-crease incision (c) and the orbital floor through inferior trans-conjunctival incision (d) to achieve orbital decompression through hidden incisions |
 |
| Figure 15: Pre- and post-operative photographs of orbital decompression for moderate (a), and severe (b) prominence of the eyes secondary to thyroid eye disease. Extent of decompression (fat and bony walls) depends upon the extent of prominence of the eyeball and is performed through hidden conjunctival incisi |
Complications
Complications of orbital decompression include orbital hematoma, strabismus, and in extreme cases, loss of vision.
Periocular injectables
Botulinum toxin injection and hyaluronic acid fillers are commonly used in the periorbital area.
Complications of Periorbital Rejuvenation
This section intends to update the dermatologist with some of the common complications that can occur in periorbital area along with preventive pearls from the ophthalmologist.
Dry eye
Treatment of crow′s feet involves botulinum toxin injection close to the lacrimal gland, which is located just within the orbital rim supero-temporally. Though gross reduction in tear secretion has not been reported, a recent study has warned injectors to be cautious in patients with diagnosed dry eye. [23]
Ptosis
Ptosis following botulinum toxin injection is due to the effect of the toxin on the muscle belly of levator palpelrae superioris muscle. The risk is highest when treating the corrugator supercilli muscle for glabellar folds. [24] The corrugator muscle being deep, botulinum toxin injection into the muscle may affect the levator muscle due to its spread along pre-periosteal spread and also due to spread along the course of superior ophthalmic vein [Figure - 1]. [24] Injecting superficially, away from the orbital rim, is the best way to avoid ptosis [Figure - 16]d. There is no effective topical medication that can be used to correct the ptosis following periocular botulinum toxin injection.
 |
| Figure 16: Narrowing of the eye aperture while smiling (a) is effectively corrected (b) by a single sub-cutaneous injection of 2 units of botulinum toxin to relax the pre-tarsal orbicularis of the lower eyelid in mid-pupillary plane (c). Injection into the corrugator should be placed away from the orbital rim (d) to avoid ptosis |
Ecchymosis and periocular hematoma
The periocular soft tissue has a rich blood supply [Figure - 1], and, therefore, is prone to bleed while injection procedures. Reducing the local temperature using ice-packs can decrease the chances of bleeding. Reclining the patient for a few minutes while preparing for the injection can help engorge prominent veins, which can then be marked and thereby avoided. While injecting the corrugator, the supra-orbital vessel pulsations can be usually felt to know its course and avoid injuring it. ′Pinching′ the soft tissue while injecting further reduces the chances of bleeding.
Despite all precautions, when a vessel is injured, it can either ooze out of the needle track or lead to a sub-cutaneous hematoma, orbital hematoma, or sub-conjunctival hemorrhage depending upon the location of the bleeding vessel. If needle track is oozing, I personally avoid compression (allowing it to flow out is better than having an ecchymosis a few days later) since it eventually stops. If a sub-cutaneous bluish swelling is beginning to appear, one should stop further injection and compress the suspected area of bleed against the firm bone of the orbital rim (rather than simply compressing it over closed eyes). A sub-conjunctival hemorrhage [Figure - 17] can be especially alarming to the dermatologist and to the patient, but it only represents a hemorrhage behind the orbital septum (post-septal tissue planes are continuous with the sub-conjunctival space). In the absence of proptosis, sub-conjunctival hemorrhage is innocuous and does not require any special treatment. A periocular/retrobulbar hematoma is the most serious consequence of a periocular bleed. In addition to swelling within the eyelid, patient can also develop proptosis. The best way to assess developing proptosis is to look for prominence of the eye in the ′up-the-nose′ view as shown in [Figure - 17]. Proptosis, if present, warrants immediate evaluation and treatment by an ophthalmologist/ophthalmic plastic surgeon.
 |
| Figure 17: Patient showing sub-conjunctival hemorrhage and lower eyelid ecchymosis, two possible complications of periocular injections (a). Sub-conjunctival hemorrhage though alarming is self-resolving and does not require any treatment. An up-the-nose view is an excellent way to detect subtle proptosis. Patient can be asked to extend the neck until glabella and the tip of the nose are in line (b). Left eye is slightly proptosed in this case |
Lower eyelid ectropion and lacrimal pump failure
Hypertropic orbicularis roll in the lower eyelid can be effectively treated with single pre-tarsal injection of 2 units of type A botulinum toxin in the mid-pupillary plane [Figure - 16]. In young individuals, ectropion of the lower eyelid is highly unlikely and is an overstated side effect. Similarly, though tear drainage has been reported to reduce following medial injections of botulinum toxin in the lower eyelid, it rarely leads to any clinically significant watering. [25]
Blindness
Partial or total blindness is the most serious ophthalmic complication of periocular filler injection. [26],[27] It is thought to occur due to retrograde intra-arterial migration of filler particles into the ophthalmic artery during the injection procedure. The filler particles then flow antegrade to get lodged into central retinal artery, which is an end-artery. The symptoms are immediate with sudden onset ocular pain and drop in vision. Slow injection, use of vasoconstrictors in the local anesthetic, and use of cannulas is recommended to reduce the risk of this rare but serious complication. [28] Once an arterial occlusion has occurred, there is no effective treatment. [29] Despite described treatment options (which need to be administered within 100 minutes), such as anterior chamber paracentesis, globe massage, and intravenous acetazolamide, the visual prognosis remains poor. A mention of this complication in the consent form, as well as measurement of visual acuity using pocket Snellens chart at the end of filler injection procedure, would be of medico-legal value to all dermatologists. It would be prudent for dermatologists who routinely perform periocular fillers to have a retinal surgeon (or ophthalmologist) available on call in the event of this rare but serious complication.
Conclusion
The periocular region is the first to reveal aging changes on the face. The upper face and mid-face can be significantly improved by minimally invasive non-surgical and surgical procedures. In practice, the rejuvenation of this complex anatomical area requires a combination of therapies including fat excision, repositioning or transfer, simultaneous brow or mid-face lift, and adjunctive treatment for skin resurfacing and periorbital hollows. The dermatologist should be aware of the surgical treatment options and also the periocular complications of non-surgical treatments, mainly injectables.
| 1. |
Castro E, Foster JA. Upper lid blepharoplasty. Facial Plast Surg 1999;15:173-81.
[Google Scholar]
|
| 2. |
Jacono AA, Moskowitz B. Transconjunctival versus transcutaneous approach in upper and lower blepharoplasty. Facial Plast Surg 2001;17:21-8.
[Google Scholar]
|
| 3. |
Lewis CD, Perry JD. A paradigm shift: Volume augmentation or 'inflation' to obtain optimal cosmetic results. Curr Opin Ophthalmol 2009;20:389-94.
[Google Scholar]
|
| 4. |
Ben Simon GJ, McCann JD. Cosmetic eyelid and facial surgery. Surv Ophthalmol 2008;53:426-42.
[Google Scholar]
|
| 5. |
Little JW. Three-dimensional rejuvenation of the midface: Volumetric resculpture by malar imbrication. Plast Reconstr Surg 2000;105:267-85.
[Google Scholar]
|
| 6. |
Rizk SS, Matarasso A. Lower eyelid blepharoplasty: Analysis of indications and the treatment of 100 patients. Plast Reconstr Surg 2003;111:1299-306.
[Google Scholar]
|
| 7. |
Zarem HA, Resnick JI. Minimizing deformity in lower blepharoplasty. The transconjunctival approach. Clin Plast Surg 1993;20:317-21.
[Google Scholar]
|
| 8. |
Adamson PA, Strecker HD. Transcutaneous lower blepharoplasty. Facial Plast Surg 1996;12:171-83.
[Google Scholar]
|
| 9. |
Zarem HA, Resnick JI. Minimizing deformity in lower blepharoplasty. The transconjunctival approach. Clin Plast Surg 1993;20:317-21.
[Google Scholar]
|
| 10. |
Zarem HA, Resnick JI. Expanded applications for transconjunctival lower lid blepharoplasty. Plast Reconstr Surg 1991;88:215-20.
[Google Scholar]
|
| 11. |
Flowers RS. Canthopexy as a routine blepharoplasty component. Clin Plast Surg 1993;20:351-65.
[Google Scholar]
|
| 12. |
Honrado CP, Pastorek NJ. Long-term results of lower-lid suspension blepharoplasty: A 30-year experience. Arch Facial Plast Surg 2004;6:150-4.
[Google Scholar]
|
| 13. |
Parkes M, Fein W, Brennan HG. Pinch technique for repair of cosmetic eyelid deformities. Arch Ophthalmol 1973;89:324-8.
[Google Scholar]
|
| 14. |
Hamra ST. Arcus marginalis release and orbital fat preservation in midface rejuvenation. Plast Reconstr Surg 1995;96:354-62.
[Google Scholar]
|
| 15. |
Baker SR. Orbital fat preservation in lower-lid blepharoplasty. Arch Facial Plast Surg 1999;1:33-7.
[Google Scholar]
|
| 16. |
Goldberg RA. Transconjunctival orbital fat repositioning: Transposition of orbital fat pedicles into a subperiosteal pocket. Plast Reconstr Surg 2000;105:743-8.
[Google Scholar]
|
| 17. |
Loeb R. Fat pad sliding and fat grafting for leveling lid depressions. Clin Plast Surg 1981;8:757-76.
[Google Scholar]
|
| 18. |
Kawamoto HK, Bradley JP. The tear ''TROUF'' procedure: Transconjunctival repositioning of orbital unipedicled fat. Plast Reconstr Surg 2003;112:1903-7.
[Google Scholar]
|
| 19. |
Patipa M. Transblepharoplasty lower eyelid and midface rejuvenation: Part I. Avoiding complications by utilizing lessons learned from the treatment of complications. Plast Reconstr Surg 2004;113:1459-68.
[Google Scholar]
|
| 20. |
Olver JM. Raising the suborbicularis oculi fat (SOOF): Its role in chronic facial palsy. Br J Ophthalmol 2000;84:1401-6.
[Google Scholar]
|
| 21. |
Sullivan SA, Dailey RA. Endoscopic subperiosteal midface lift: Surgical technique with indications and outcomes. Ophthal Plast Reconstr Surg 2002;18:319-30.
[Google Scholar]
|
| 22. |
Goldberg RA. Advances in Surgical Rehabilitation in Thyroid Eye Disease. Thyroid 2008;18:989-95.
[Google Scholar]
|
| 23. |
Arat YO, Yen MT. Effect of botulinum toxin type a on tear production after treatment of lateral canthal rhytids. Ophthal Plast Reconstr Surg 2007;23:22-4.
[Google Scholar]
|
| 24. |
Ramey NA, Woodward JA. Mechanisms of blepharoptosis following cosmetic glabellar chemodenervation. Plast Reconstr Surg 2010;126:248-49.
[Google Scholar]
|
| 25. |
Sahlin S, Chen E, Kaugesaar T, Almqvist H, Kjellberg K, Lennerstrand G. Effect of eyelid botulinum toxin injection on lacrimal drainage. Am J Ophthalmol 2000;129:481-6.
[Google Scholar]
|
| 26. |
Peter S, Mennel S. Retinal branch artery occlusion following injection of hyaluronic acid (Restylane). Clin Experiment Ophthalmol 2006;34:363-4.
[Google Scholar]
|
| 27. |
Roberts SA, Arthurs BP. Severe visual loss and orbital infarction following periorbital aesthetic poly-(L)-lactic acid (PLLA) injection. Ophthal Plast Reconstr Surg 2012;28:e68-70.
[Google Scholar]
|
| 28. |
Coleman SR. Avoidance of arterial occlusion from injection of soft tissue fillers. Aesthet Surg J 2002;22:555-7.
[Google Scholar]
|
| 29. |
Körner-Stiefbold U. Central retinal artery occlusion--etiology, clinical picture, therapeutic possibilities. Ther Umsch 2001;58:36-40.
[Google Scholar]
|





