Translate this page into:
Mucocutaneous manifestations in children with human immunodeficiency virus infection
Correspondence Address:
Vibhu Mendiratta
Department of Dermatology, Lady Hardinge Medical College and Associated Hospitals, Shahid Bhagat Singh Marg, New Delhi - 110 001
India
| How to cite this article: Mendiratta V, Mittal S, Jain A, Chander R. Mucocutaneous manifestations in children with human immunodeficiency virus infection. Indian J Dermatol Venereol Leprol 2010;76:458-466 |
Abstract
Skin is one of the most frequently involved organs in human immunodeficiency virus (HIV) infection, and mucocutaneous manifestations may be one of the earliest markers of AIDS. The prevalence of cutaneous abnormalities in HIV approaches nearly 90%. Mucocutaneous manifestations may also act as a prognostic marker of HIV infection. Children are increasingly being affected by HIV infection and it is important to realize the presence of the infection early in the disease process as their immune status is not mature enough to handle the stress of various infections. Skin manifestations can serve as early markers and prognostic indicators of HIV infection. This review highlights the epidemiology, transmission, pathogenesis, and the mucocutaneous manifestations of HIV infection in children.Introduction
Human immunodeficiency virus (HIV) infection in children is becoming a common occurrence. In children, it is largely a preventable disease. Skin manifestations constitute one of the most common clinical features in such children and their clinical pattern and severity is more or less in accordance with their CD 4 counts. Thus an early recognition of such features is important for an early diagnosis and also to assess the prognosis of HIV infection. Children with HIV infection are more prone to adverse cutaneous drug reactions, both to anti-retroviral therapy (ART) and to other drugs that are given concomitantly for co-morbid illnesses.
The first pediatric case of AIDS was reported to the Centre for Disease Control and Prevention (CDC) in November 1982. Globally, there were a total of 33.2 million people living with HIV, in 2007, of which 2.5 million (7.5%) were children under the age of 15 years. [1] Total number of deaths was 2.1 million, of which 330,000 were children. It is estimated that more than 90% of children living with HIV acquired the virus during pregnancy, birth, or breastfeeding, forms of HIV transmission that can be prevented. [2]
In 2007, it is estimated that there are 2.31 million (1.8-2.9 million) people living with HIV/AIDS in India (making it the third largest country with regard to the number of people with HIV) with an estimated adult HIV prevalence of 0.34% (0.25-0.43%). Out of the estimated number of PLHA (people living with HIV/AIDS), 39% are females and 3.5% are children. [3]
Transmission of HIV can occur in following three ways:
- Sexual route
- Contaminated blood and body fluids
- Vertical transmission
HIV infection in children occurs mainly through vertical transmission, i.e. from mother to child. The risk of transmission by an infected mother occurring before or during birth (without interventions to reduce transmission) is 15-25%. Breastfeeding by an infected mother increases the risk by 5-20% to a total of 20-45%. [4] In a study done in Brazil, vertical transmission was seen in 97.5% of children. [5] Various studies done in India have reported vertical transmission as a cause of pediatric HIV in 51-83% of cases. [6],[7],[8]
Pathogenesis
HIV infection is characterized by an insidious deterioration of the cellular immune system. The degree of immunodeficiency associated with HIV infection, as defined by the onset of opportunistic diseases, correlates closely with plasma CD 4 T-cell counts.
HIV enters into the CD 4 T-cells by the process of binding and fusion. It synthesizes DNA from its RNA with the help of reverse transcriptase, which then integrates into the host DNA and undergoes transcription. The new protein thus formed assembles into a new virion which is released by budding and goes on to infect the other CD 4 T cells. [9]
Approximately 100 billion new viral particles are produced every day, and 1 to 2 billion CD 4 T cells die each day. [10] This depleted pool of CD 4 T cells is not completely replaced and the host thus remains deficient in CD 4 T cells. Although marked reduction in CD 4 T cells can account for most of the immunodeficiency, there is evidence that qualitative defects in T cells can be detected even in asymptomatic individuals. [11]
Clinical Features
HIV is a multi-system infection affecting virtually every organ of the body. HIV infection produces a spectrum of illness from totally asymptomatic infection to AIDS.
Patterns of disease expression and progression differ among HIV infected children. [12] Most children with HIV infection acquired from the mother will display features of the infection within 6 months of life, [13] whereas some remain asymptomatic till the age of 8-10 years. [14] The onset of HIV infection in children has a wide spectrum of clinical manifestations. [13]
Some infants present with features of severe immunodeficiency, whereas others have non-specific findings such as hepatosplenomegaly, failure to thrive, unexplained persistent fever, parotitis, and recurrent gastroenteritis. During the first year, lymphadenopathy, splenomegaly, and hepatomegaly, singularly or combined, have been observed in more than 50% of children; other signs including failure to thrive, fever, diarrhea, and AIDS defining secondary infections, are frequently observed, but can also present at a later age. [14]
Cutaneous Manifestations
Skin is commonly involved in HIV infection and nearly 90% of patients with HIV infection have dermatological manifestations at some stage during the course of their disease. [15],[16]
The data currently with regard to the mucocutaneous manifestations of HIV infection in pediatric population come mainly from the western literature. The prevalence of mucocutaneous manifestations in children with HIV infection, from various parts of the world, is highly variable, ranging from as low as 42% to almost 93%. [8],[17],[18],[19],[20],[21]
In India, skin manifestations among HIV-infected children show a prevalence rate varying from 30 to 80%. [10],[22],[23] HIV-infected children often present with common childhood infections. These, however, tend to be more severe, may manifest atypically, are often resistant to treatment, and tend to have a high rate of recurrence. The various clinical manifestations seen in children are tabulated in [Table - 1]. [24]

Infections
Fungal infections
Candidiasis: Candidiasis is one of the most common mucocutaneous manifestations of HIV infection in children, and its incidence has been estimated to range between 20% to 72%. [15],[17],[25],[26] Oral involvement is the most common [Figure - 1]a presentation of which can be as: (1) pseudomembranous (thrush), (2) erythematous (atrophic), (3) papillary hyperplasia, (4) chronic hyperplastic, (5) angular cheilitis, and (6) median rhomboid glossitis. It has been suggested in several studies that thrush is a marker of rapid HIV disease progression and death. [25],[26] Although it can occur without severe cell depletion, it is more commonly seen with low CD 4 counts or symptomatic HIV disease. The manifestations in an HIV positive differ from those in an immuno-competent child by persistence beyond the age of 6 months, the presence of severe or recurrent episodes, and the coexistence of lymphadenopathy, splenomegaly, or wasting syndrome. [27],[28] Candida albicans is the usual pathogen causing oral candidiasis, but other strains can occasionally be isolated. [29]
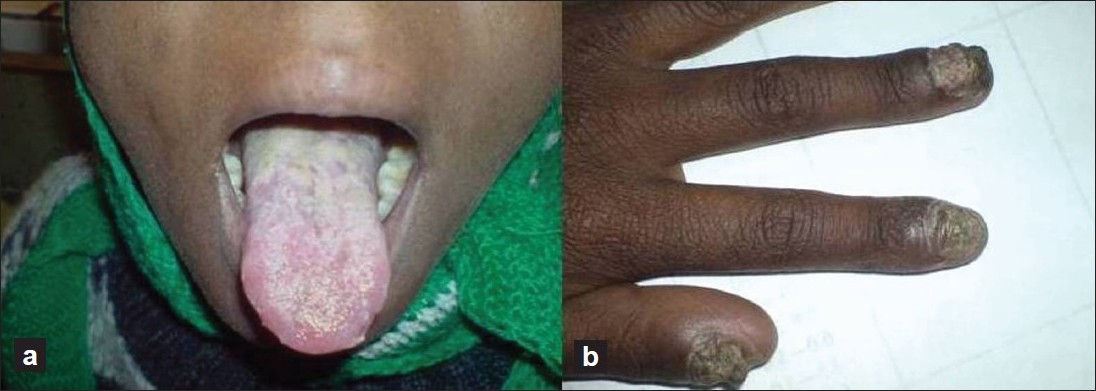 |
| Figure 1 :(a) Oral candidiasis (thrush). (b) Onychomycosis (total) |
Dermatophytosis: Infection by dermatophytes occurs with an increased frequency and aggressiveness in HIV-infected patients. Tinea corporis, tinea capitis, tinea faciale, and onychomycosis [Figure - 1]b are particularly common. [15],[30] Cases of severe (such as kerion) and recurrent tinea capitis have been observed. [28] Proximal white subungual onychomycosis of fingernails, periungual involvement, and rapid spreading of the infection to involve all 10 finger and toenails are common findings in HIV-infected individuals with low CD 4 cell counts. [31] Dermatophytic infections are particularly resistant to topical agents, and recurrences after topical and systemic therapy are common.
Deep fungal infections:Histoplasma capsulatum, Coccidiodes immitis, Aspergillus fumigatus, Malassezia furfur, Sporothrix schenckii, and others can cause opportunistic infections in HIV-infected adults, [32] but are rarely observed in HIV-infected children. [30] Disseminated sporotrichosis with painful ulcers has been described in children. Sirisanthana et al0.,[33] reported a series of 21 HIV-infected children with disseminated Penicillium marneffei infection. Papular skin lesions with central umbilication on the face and extremities appeared in 67% of patients and provided the most significant clue to the diagnosis. The disease occurs late in the course of HIV infection.
Bacterial infections
Pyodermas:Generally, children manifest recurrent bacterial infections rather than primary opportunistic ones as seen in adults. [27] The most common isolates are Streptococcus pneumoniae, Haemophilus influenzae type B, and Salmonella species. [27],[30] Staphylococcal infections are the most common skin infections, usually presenting as cellulitis, ecthyma, erysipelas, furunculosis (occasionally of disseminated nature), persistent and recurrent folliculitis, and impetigo. [17],[30],[32],[34]
Bacillary angiomatosis: Although the disease has been described in immunocompetent children, [35] it is rarely seen in HIV-infected children. The etiologic agent is Bartonella henselae and B. quintana. Lesions begin as small, erythematous, vascular papules that may enlarge to form exophytic, friable nodules surrounded by a collarette of scale with or without erythema.
Mycobacterial infections: HIV-infected children are at an increased risk of tuberculosis but cutaneous involvement is not a common occurrence. Mycobacterium avium intracellular complex (MAC) is one of the most frequent atypical mycobacterial infections in HIV-infected patients. Skin is rarely infected, and children with late stage disease (CD 4 <100 cells/mm 3 ) are more prone. Cutaneous abscesses, macular lesions, and perianal ulcerations have been reported in HIV-infected adults but may also occur in pediatric cases. [36] A large prospective done over a population of 1, 52, 000 adult patients revealed no differences in the incidence, presentation, or severity of cutaneous tuberculosis in HIV-positive patients. [37]
Viral infections
Chicken pox: Varicella may run a prolonged course (>10 days) in HIV-infected children, [38] and persistent and recurrent infections are particularly problematic. Von Seidlein et al.[39] documented an association between increasing numbers of episodes of VZV infection and a low CD 4 count at the time of primary infection.
Herpes zoster: Herpes zoster (HZ) is rare in immunocompetent children but occurs with increased frequency in HIV-infected children. In addition to classic papulovesicular HZ, persistent ulcerative and disseminated forms [Figure - 2] may be observed. [40] Von Seidlein et al0.,[39] documented that the presentation of zoster as the first recurrence of VZV infection is associated with low CD 4 counts.
Herpes simplex virus: HSV infection correlates primarily with CD 4 cell counts. The most common feature of HSV in pediatric HIV infection is herpetic gingivostomatitis, [41] with painful, recurrent, or chronic ulcerations of the lips, tongue, palate, and buccal mucosa. [42] The frequency of herpetic gingivostomatitis is especially high in those with CD 4 counts <50 cells/mm 3.
Human papilloma virus: HPV may cause verruca vulgaris, widespread flat warts, and condylomata acuminata. Warts can be single but usually are multiple. [15],[28],[30] Extensive anogenital warts, very resistant to treatment, have also been observed. [43] Epidermodysplasia verruciformis, an HPV infection caused by HPV types 5 and 8, is an autosomal recessive disorder and has been known to occur in association with many immunodeficient states including HIV. [44]
 |
| Figure 2 :Multidermatomal herpes zoster involving L2, L3, and L4 segments |
Molluscum contagiosum: In children with HIV infection, it often involves atypical areas, such as the face and neck [15],[34] and tend to be more confluent and occasionally extremely numerous. [15],[36],[42] In addition, giant lesions (>1 cm) may occur. [15],[36],[42] Lim et al.[17] noted that unusual features may occur without severe CD 4 cell depletion. In contrast to the usual course in healthy children, molluscum lesions in HIV-infected patients tend to persist.
Measles: In developing countries, measles has been reported to run a more severe course in HIV-infected children, with estimated fatality rates of 40-70%. [45] The increased mortality has been attributed to a higher rate of measles giant cell pneumonia. Some of the children do not manifest the typical measles exanthem. [46]
Cytomegalovirus infection: In AIDS patients, the most common lesions reported to contain CMV have been ulcerations of the orofacial or perineal area. [47]
Epstein-Barr virus: Oral hairy leukoplakia, characterized by discrete, whitish patches with parallel vertical ridges on the lateral border of the tongue, has been reported to occur rarely in HIV-infected children. [15],[48]
Infestations
Scabies: Independently of CD 4 counts, most patients have scabetic burrows at characteristic sites, such as the wrists and finger web spaces. Patients with CD 4 counts <150 cells/mm 3 may present with crusted Norwegian scabies. [17],[42] The infestation might be particularly resistant to treatment.
Pediculosis and demodicosis: Pediculosis is particularly common, especially in children with low socio-economic status. [15] Papular lesions on the face of two HIV-infected children in relation to Demodex mites have been described. [49] The main defense against Demodex mites are the CD 4 cells, which are defective in HIV infection.
Inflammatory dermatoses
Pruritic papular eruption (PPE): PPE is often one of the earliest manifestations of HIV infection and is a useful cutaneous marker for immune status in such patients. [50] The concentration of the lesions is highest on the extremities [Figure - 3], but the trunk and face are also involved in half of the patients. [51] It is a sign of waning immunity in these patients, and usually occurs at counts <50 cells/mm 3.[51]
 |
| Figure 3 :Multiple discrete reddish-brown excoriated papules involving the extremities |
Seborrheic dermatitis (SD): It is possibly one of the most common cutaneous manifestations of HIV disease, its incidence ranging from 32 to 83%. [52] In children with HIV infection, SD seems to occur with increased frequency. [17] Its severity has been correlated with the degree of HIV-related immunodeficiency and the CD 4 cell count. [17],[27] In infants, the disorder may take the form of severe erythema and scaling of the face, scalp, and diaper area, sometimes progressing to erythroderma. [28],[36]th
Atopic dermatitis: Parkin et al.[53] documented the association of atopic manifestations with established AIDS. Atopic dermatitis appears to be triggered by HIV sero-conversion in genetically predisposed individuals. In certain series, atopic dermatitis does not seem to be more frequent in seropositive children than in the healthy population. [15]
Psoriasis: In adults with HIV infection, psoriasis may appear suddenly and with extreme severity, while it is subject to precipitous flares and resistance to treatment. [54] Both plaque and guttate psoriasis in children and adolescents with HIV infection have been observed. [15],[28]th
Drug eruptions: Patients with HIV disease are particularly prone to hypersensitivity drug eruptions. Hachem et al.[15] reported an incidence of 12% of drug-related rashes among 85 HIV-infected children. It is seen as morbilliform skin eruptions appearing 8-10 days after initiation of therapy [Figure - 4] and resolving quickly after discontinuation of the drug. Dusky erythematous macules, [55] Stevens-Johnson syndrome, [28] and toxic epidermal necrolysis [42] may also occur. Co-trimoxazole, ampicillin and antituberculous medication are other agents frequently implicated in drug eruptions. [30]
 |
| Figure 4 :Nevirapine induced morbilliform rash |
Vasculitis: Leukocytoclastic vasculitis may develop as a result of drug reaction, concomitant infection, or HIV infection itself. Chren et al.[56] reported a 9-year-old girl with persistent, palpable purpura of the lower extremities as the sole manifestation of HIV infection. Three children with vasculitic lesions resembling cutis marmorata have also been reported. [57] Other vascular phenomena known to occur in children with HIV infection are splinter hemorrhages, telangiectasias, and immune thrombocytopenia. [17]th
Neoplastic conditions
Kaposi′s sarcoma (KS): KS is rare in children. [58] KS in children points to a nonsexual mode of transmission. HHV-8 can be acquired as a common childhood infection [59] and may possibly be horizontally transmitted from mother to child [60] during birth or breastfeeding. There is a male preponderance for childhood HIV-related KS, and the median age of presentation is 4 years. Clinically, it may look like a red, bluish, or brownish macule, papule, small plaque, or a smooth raised tumor. Lesions may appear anywhere on the skin including palms, soles, body folds, ears, scalp, and mucosal surfaces, particularly the hard palate.
Non-Hodgkin lymphoma (NHL): NHL is more common in children and adolescents with AIDS. An important role for Epstein-Barr virus has been suggested, and all children have low CD 4 counts at the time of diagnosis. In a British study, seven cases of NHL were identified among 302 HIV-infected children. [61]
Hair and Nail changes
Hair abnormalities: Hair changes such as hypertrichosis of the eyelashes, thinning of hair, premature graying, telogen effluvium, and alopecia (due to severe SD, malnutrition or unknown causes) have been reported to occur in HIV infection. [34],[45]th
Nail abnormalities: Nail changes such as yellow discoloration, transverse or longitudinal ridging, paronychia, onychomycosis, etc. have been described in association with HIV infection. [34],[45] These can occur either primarily or secondary to infections or anti-retroviral drugs given.
Miscellaneous
Alopecia due to severe seborrheic dermatitis, [17] nutritional deficiency, or unknown causes may be observed in the HIV-infected pediatric population. [15],[17]
An exanthematous eruption associated with the flulike syndrome of primary HIV infection has been documented in adults. [42] A similar rash has been reported in 33% of 82 HIV-infected children from Uganda. [62]HIV-infected children are more vulnerable to abuse. A peculiar annular eruption in a 7-year-old girl finally proved to be the result of the abusive behavior of her adoptive parent. [63]
Manifestations due to anti-retroviral therapy
Two regimens of ART are currently followed: the first regimen utilizes two nucleoside analogs (one of which is usually lamivudine) and a non-nucleoside reverse transcriptase inhibitor. The second regimen utilizes two nucleoside analogs and a protease inhibitor. Initiation of ART in children is guided by child′s WHO clinical stage as well as the CD 4 count, taken together [Table - 2].

The advent of HAART (highly active anti-retroviral therapy) or combined ART has changed the spectrum of skin disorders by improving host immunity. HIV-infected patients are more likely, than the general population to suffer from adverse drug reactions. HAART, with no exception, carries the risk in causing mucocutaneous adverse reactions [Table - 3]. [64],[65]

IRIS
Another event seen in children on ART is immune reconstitution inflammatory syndrome (IRIS). It is defined as "a collection of signs and symptoms resulting from the ability to mount an immune response to antigens or organisms associated with immune recovery on ART." [66] It is seen more commonly in those with severe immunodeficiency and presents most commonly within 2-12 weeks of initiating ART. It presents as an unexpected deterioration of clinical status soon after commencing ART. Sub-clinical infections, such as TB, are unmasked, which present as new active disease and there may even be development of abscess at the BCG vaccination site. Most common IRIS events seen are M. tuberculosis, herpes zoster and cryptococcal disease.
Conclusions
Skin manifestations are a common occurrence in HIV-infected children and their pattern can help predict the severity of the disease. The type and the characteristics of various mucocutaneous disorders seen in HIV co-relate well with the CD 4 counts and can help predict the degree of immunodeficiency with fair precision. Such knowledge is especially helpful in resource poor countries like ours where availability of CD 4 counts is limited.
| 1. |
UNAIDS and WHO. AIDS epidemic update. December 2007.
[Google Scholar]
|
| 2. |
UNAIDS. Report on the global AIDS epidemic. August 2008.
[Google Scholar]
|
| 3. |
Ministry of Health and Family Welfare. HIV Sentinel Surveillance and HIV Estimation in India 2007 A Technical Brief. NACO October 2008.
[Google Scholar]
|
| 4. |
WHO. HIV transmission through breast feeding: A review of available evidence. 2004.
[Google Scholar]
|
| 5. |
De Carvalho VO, Marinoni LP, Martins LT, Giraldi S, Taniguchi K, Bertogna J. Dermatological alterations in children with AIDS and their relation to clinical-immunological categories and viral load. An Bras Dermatol 2003;78:679-92.
[Google Scholar]
|
| 6. |
Sehgal R, Baveja UK, Chattopadhya D, Chandra J, Lal S. Pediatric HIV infection. Indian J Pediatr 2005;72:925-30.
[Google Scholar]
|
| 7. |
Madhivanan P, Mothi SN, Kumarasamy N, Yepthomi T, Venkatesan C, Lambert JS, et al. Clinical manifestations of HIV infected children. Indian J Pediatr 2003;70:615-20.
[Google Scholar]
|
| 8. |
Shah I. Age related clinical manifestations of HIV infection in Indian children. J Trop Pediatr 2005;51:300-3.
[Google Scholar]
|
| 9. |
Abbas AK. Diseases of immunity. In: Kumar V, editor. Robbins and Cotran Pathologic Basis of Disease. 7 th ed. India: Elsevier; 2004. p. 248-58.
[Google Scholar]
|
| 10. |
Haase AT. Population biology of HIV-1 infection: Viral and CD4+ T cell demographics and dynamics in lymphoid tissues. Annu Rev Immunol 1999;17:625-56.
[Google Scholar]
|
| 11. |
Greene WC, Peterlin BM. Charting HIV's remarkable voyage through the cell: Basic science as a passport to future therapy. Nat Med 2002;8:673-80.
[Google Scholar]
|
| 12. |
Tovo PA, De Martino M, Gabiano C, Cappello N, D'Elia R, Loy A, et al. Prognostic factors and survival in children with perinatal HIV-1 infection. Lancet 1992;339:1249-53.
et al. Prognostic factors and survival in children with perinatal HIV-1 infection. Lancet 1992;339:1249-53.'>[Google Scholar]
|
| 13. |
Natural history of vertically acquired human immunodeficiency virus-1 infection. The European Collaborative Study. Pediatrics 1994;94:815-9.
[Google Scholar]
|
| 14. |
Scarlatti G. Pediatric HIV infection. Lancet 1996;348:863-8.
[Google Scholar]
|
| 15. |
El Hachem M, Bernardi S, Pianosi G, Krzysztofiak A, Livadiotti S, Gattinara GC. Mucocutaneous manifestations in children with HIV infection and AIDS. Pediatr Dermatol 1998;15:429-34.
[Google Scholar]
|
| 16. |
Cockerell C, Friedman-Klein A. Cutaneous signs of HIV infection. Clin Dermatol 1993;4:507-24.
[Google Scholar]
|
| 17. |
Lim W, Sadick N, Gupta A, Kaplan M, Pahwa S. Skin diseases in children with HIV infection and their association with degree of immunosuppression. Int J Dermatol 1990;29:24-30.
[Google Scholar]
|
| 18. |
Wananukul S, Deekajorndech T, Panchareon C, Thisyakorn U. Mucocutaneous findings in pediatric AIDS related to degree of immunosuppression. Pediatr Dermatol 2003;20:289-94.
[Google Scholar]
|
| 19. |
Wananukul S, Thisyakorn U. Mucocutaneous manifestations of HIV infection in 91 children born to HIV seropositive women. Pediatr Dermatol 1999;16:359-63.
[Google Scholar]
|
| 20. |
Co M, Sadick N, Ravipati M, Kaplan E, Pahwa S. Mucocutaneous manifestations of HIV in children and their correlation with immunosuppression. Int Conf AIDS 1990;6:219.
[Google Scholar]
|
| 21. |
El Hachem M, Castelli G, Pianosi G, Krzysztofiak A, Livadiotti S, Ferri M. HIV infection in children: Mucocutaneous manifestations. Int Conf AIDS 1994;10:262.
[Google Scholar]
|
| 22. |
Pol RR, Shepur TA, Ratageri VH. Clinico-laboratory profile of pediatric HIV in Karnataka. Indian J Pediatr 2007;74:1071-5.
[Google Scholar]
|
| 23. |
Shah SR, Tullu MS, Kamat JR. Clinical profile of pediatric HIV infection from India. Arch Med Res 2005;36:24-31.
[Google Scholar]
|
| 24. |
Stefanaki C, Stratigos AJ, Stratigos JD. Skin manifestations of HIV-1 infection in children. Clin Dermatol 2002;20:74-86.
[Google Scholar]
|
| 25. |
European Collaborative Study. Children born to women with HIV-1 infection: Natural history and risk of transmission. Lancet 1991;337:253-60.
[Google Scholar]
|
| 26. |
Kline MW. Oral manifestations of pediatric human immunodeficiency virus infection: A review of the literature. Pediatrics 1996;97:380-8.
[Google Scholar]
|
| 27. |
Zuckerman G, Metrou M, Bernstein LJ, Crain EF. Neurologic disorders and dermatologic manifestations in HIV infected children. Pediatr Emerg Care 1991;7:99-105.
[Google Scholar]
|
| 28. |
Prose NS. Skin manifestations of HIV-1 infection in children. Clin Dermatol 1991;9:59-64.
[Google Scholar]
|
| 29. |
Flynn PM, Cunningham CK, Kerkering T, San Jorge AR, Peters VB, Pitel PA, et al. Oropharyngeal candidiasis in immunocompromised children: A randomized, multicenter study of orally administered fluconazole suspension versus nystatin. The Multicenter Fluconazole Study Group. J Pediatr 1995;127:322-8.
[Google Scholar]
|
| 30. |
Whitworth JM, Janniger CK, Oleske JM, Schwartz RA. Cutaneous manifestations of childhood acquired immunodeficiency syndrome and human immunodeficiency virus infection. Cutis 1995;55:62-6, 70-2.
[Google Scholar]
|
| 31. |
Daniel RC, Norton LA, Scher RK. The spectrum of nail disease in patients with human immunodeficiency virus infection. J Am Acad Dermatol 1992;27:93-7.
[Google Scholar]
|
| 32. |
Domachowske JB. Pediatric human immunodeficiency virus infection. Clin Microbiol Rev 1996;9:448-68.
[Google Scholar]
|
| 33. |
Sirisanthana V, Sirisanthana T. Disseminated Penicillium marneffei infection in human immunodeficiency virus infected children. Pediatr Infect Dis J 1995;14:935-40.
[Google Scholar]
|
| 34. |
Straka BF, Whitaker DL, Morrison SH, Oleske JM, Grant-Kels JM. Cutaneous manifestations of AIDS in children. J Am Acad Dermatol 1988;18:1089-102.
[Google Scholar]
|
| 35. |
Paul MA, Fleischer AB Jr, Wieselthier JS, White WL. Bacillary angiomatosis in an immunocompetent child: The first reported case. Pediatr Dermatol 1994;11:338-41.
[Google Scholar]
|
| 36. |
Prose NS. Mucocutaneous disease in pediatric human immunodeficiency virus infection. Pediatr Clin North Am 1991;38:977-90.
[Google Scholar]
|
| 37. |
Arora S, Arora G, Kakkar S. Cutaneous tuberculosis: A clinico-morphological study. Med J Armed Forces India 2006;62:344-7.
[Google Scholar]
|
| 38. |
Leibovitz E, Cooper D, Giurgiutiu D, Coman G, Straus I, Orlow SJ, et al. Varicella zoster virus infection in Romanian children infected with the human immunodeficiency virus. Pediatrics 1993;92:838-42.
[Google Scholar]
|
| 39. |
Von Seidlein L, Gillette SG, Bryson Y, Frederick T, Mascola L, Church J, et al. Frequent recurrence and persistence of varicella-zoster virus infections in children infected with human immunodeficiency virus type 1. J Pediatr 1996;128:52-7.
[Google Scholar]
|
| 40. |
Grossman MC, Grossman ME. Chronic hyperkeratotic herpes zoster and human immunodeficiency virus infection. J Am Acad Dermatol 1993;28:306-8.
[Google Scholar]
|
| 41. |
Berger T. Herpes virus infections and HIV disease. Clin Dermatol 1991;9:79-85.
[Google Scholar]
|
| 42. |
Prose NS. HIV infection in children. J Am Acad Dermatol 1990;22:1223-31.
[Google Scholar]
|
| 43. |
Laraque D. Severe anogenital warts in a child with HIV infection. N Engl J Med 1989;320:1220-1.
[Google Scholar]
|
| 44. |
Hu W, Nuovo G, Willen M, Somach S. Epidermodysplasia Verruciformis in two half brothers with HIV Infection. J Cutan Med Surg 2004;8:357-60.
[Google Scholar]
|
| 45. |
Dray-Spira R, Lepage P, Dabis F. Prevention of infectious complications of pediatric HIV infection in Africa. AIDS 2000;14:1091-9.
[Google Scholar]
|
| 46. |
Centers for Disease Control and Prevention. Epidemiologic notes and reports-Measles in HIV-infected children. United States, Morbidity and Mortality Weekly Report 1988;37(12):183-6.
[Google Scholar]
|
| 47. |
Thiboutot DM, Beckford A, Mart CR, Sexton M, Maloney ME. Cytomegalovirus diaper dermatitis. Arch Dermatol 1991;127:396-8.
[Google Scholar]
|
| 48. |
Greenspan JS, Mastrucii MT, Legott PJ, Freese UK, De Souza YG, Scott GB, et al. Hairy leukoplakia in a child. AIDS 1988;2:143.
[Google Scholar]
|
| 49. |
Sanchez-Viera M, Hernanz JM, Sampelayo T, Gurbindo MD, Lecona M, Soto-Melo J. Granulomatous rosacea in a child infected with the human immunodeficiency virus. J Am Acad Dermatol 1992;27:1010-1.
[Google Scholar]
|
| 50. |
Liautaud B, Pape JW, DeHovitz JA, Thomas F, LaRoche AC, Verdier RI, et al. Pruritic skin lesions. A common initial presentation of acquired immunodeficiency syndrome. Arch Dermatol 1989;125:629-32.
[Google Scholar]
|
| 51. |
Bason MM, Berger TG, Nesbitt LT Jr. Pruritic papular eruption of HIV-disease. Int J Dermatol 1993;32:784-9.
[Google Scholar]
|
| 52. |
Cockerell CJ. Seborrheic dermatitis-like and atopic dermatitis-like eruptions in HIV infected patients. Clin Dermatol 1991;9:49-51.
[Google Scholar]
|
| 53. |
Parkin JM, Eales LJ, Galazka AR, Pinching AJ. Atopic manifestations in the acquired immunodeficiency syndrome: Response to recombinant interferon therapy. Br Med J 1987;294:1185-6.
[Google Scholar]
|
| 54. |
Shupack JL, Stiller MJ, Haber RS. Psoriasis and Reiter's syndrome. Clin Dermatol 1991;9:53-8.
[Google Scholar]
|
| 55. |
Rico MJ, Kory WP, Gould EW, Penneys NS. Interface dermatitis in patients with acquired immunodeficiency syndrome. J Am Acad Dermatol 1987;16:1209-18.
[Google Scholar]
|
| 56. |
Chren MM, Silverman RA, Sorensen RU, Elmets CA. Leucocytoclastic vasculitis in a patient infected with human immunodeficiency virus. J Am Acad Dermatol 1989;21:1161-4.
[Google Scholar]
|
| 57. |
Torre D, Sampietro C, Fiori GP, Dietz A, Montanari M. Skin manifestations in infants with AIDS. Int J Dermatol 1987;26:459-60.
[Google Scholar]
|
| 58. |
Orlow SJ, Cooper DC, Petrea S, Kamino H, Popescu V, Lawrence R, et al. AIDS associated Kaposi's sarcoma in Romanian children. J Am Acad Dermatol 1993;28:449-53.
[Google Scholar]
|
| 59. |
Kasolo FC, Mpabalwani E, Gompels UA. Infection with AIDS related herpesviruses in human immunodeficiency virus negative infants and endemic childhood Kaposi's sarcoma in Africa. J Gen Virol 1997;78:847-55.
[Google Scholar]
|
| 60. |
He J, Bhat G, Kansaka C, Chintu C, Mitchell C, Duan W,et al. Seroprevalence of human herpesvirus 8 among Zambian women of childbearing age without Kaposi's sarcoma (KS) and mother-child pairs with KS. J Infect Dis 1998;178:1787-90.
[Google Scholar]
|
| 61. |
Evans JA, Gibb DM, Holland FJ, Tookey PA, Pritchard J, Ades AE. Malignancies in UK children with HIV infection acquired from mother to child transmission. Arch Dis Child 1997;76:330-3.
[Google Scholar]
|
| 62. |
Ziegler JL, Katongole-Mbidde E. Kaposi's sarcoma in childhood: An analysis of 100 cases from Uganda and relationship to HIV infection. Int J Cancer 1996;65:200-3.
[Google Scholar]
|
| 63. |
Solomon BA, Laude T. A peculiar annular eruption in a child with AIDS. J Am Acad Dermatol 1995;33:513-4.
[Google Scholar]
|
| 64. |
Ward HA, Russo GG, Shrum J. Cutaneous manifestations of antiretroviral therapy. J Am Acad Dermatol 2002;46:284-93.
[Google Scholar]
|
| 65. |
Kong HH, Myers SA. Cutaneous effects of highly active antiretroviral therapy in HIV-infected patients. Dermatol Ther 2005;18:58-66.
[Google Scholar]
|
| 66. |
Ministry of Health and Family Welfare. Guidelines for HIV care and treatment in infants and children. NACO 2006. p. 85.
[Google Scholar]
|
Fulltext Views
4,547
PDF downloads
1,980





