Translate this page into:
Study of histamine wheal suppression by dexamethasone with and without iontophoresis
2 Deparment of Community Medicine, PSG Institute of Medical Sciences and Research, Coimbatore - 641 004, Tamil Nadu, India
Correspondence Address:
C R Srinivas
Department of Dermatology, PSG Hospitals, Peelamedu, Coimbatore-641 004, Tamil Nadu
India
| How to cite this article: S, Rai R, Shanmuga SV, K, Prabhu S, Srinivas C R, Mathew AC. Study of histamine wheal suppression by dexamethasone with and without iontophoresis. Indian J Dermatol Venereol Leprol 2006;72:283-285 |
Abstract
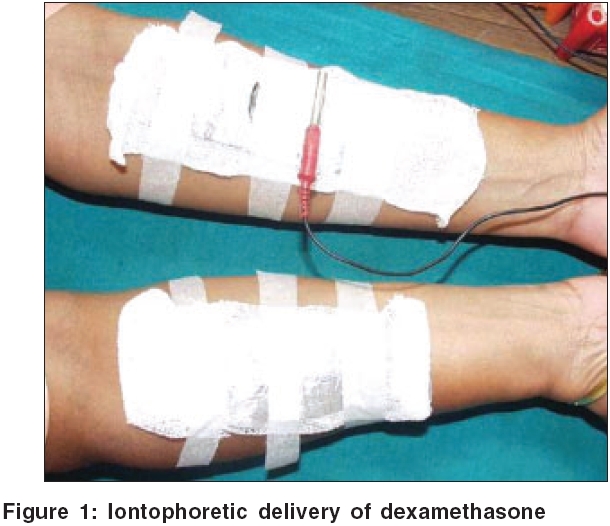
Background: Iontophoresis increases the penetration of drugs into the skin by electric current. The ability of topical steroids to reduce the size of the histamine wheal was used to assess the efficacy of topical dexamethasone delivered with and without iontophoresis. Aim: To determine the wheal suppressing ability of dexamethasone delivered with and without iontophoresis. Methods: A template with three squares of 3 x 3 cm was placed on both forearms of 20 volunteers and the edges marked. A gauze piece soaked in 2 ml of dexamethasone solution was placed on the flexor aspect of the left forearm and the electrode, an aluminum foil was placed on it and connected to the negative pole (since dexamethasone is negatively charged). An electric current was passed for 15 minutes. Similarly, on the right forearm, a dexamethasone soaked gauze piece was placed without iontophoresis. Histamine wheal suppression was assessed at the end of 30 min, 1 hr and 2 hrs, on both sides. Statistical analysis was done using an independent t-test. Results: There was a statistically significant difference in wheal suppression at 30 min ( p =0.006) on the left hand where iontophoresis was used. Conclusion: Our experiment showed that topical dexamethasone with iontophoresis has the maximum effect at the end of 30 minutes and is more effective than dexamethasone without iontophoresis.

 |
 |
 |
 |
Introduction
Drugs in ionic form have little penetration into the skin when applied topically.[1] Iontophoresis is the process of facilitating the transport of ionic drugs into the skin by using an electric current.[2] The drug is placed under the electrode with the same charge (active electrode) and the electrode with the opposite charge (passive electrode) is placed elsewhere on the skin. When an electric current is passed, the repulsive force drives the drug into skin through the eccrine glands.[3] A high concentration of a drug is delivered to a limited area by this technique.
Although steroids are available as topical preparations, their action is limited to the skin and subcutaneous tissue. Iontophoresis however, leads to increased perfusion of drug into deeper tissues and hence can be used to treat deeper structures such as joints and muscles. The oral and parenteral delivery of steroids can be associated with side effects, which can be minimized by iontophoresis. The penetration of topical dexamethasone into the skin can be increased by iontophoresis and hence it can be used for dermatological conditions. The ability of topical steroids to suppress the histamine-induced wheal has been used to assess their efficacy.[4] We compared the wheal- suppressing ability of dexamethasone delivered by iontophoresis to that without iontophoresis.
Methods
Twenty informed human volunteers (interns and staff) who had not used systemic or topical steroids and antihistamines for at least 8 weeks, were studied. Individuals with a history of atopy were excluded from the study.
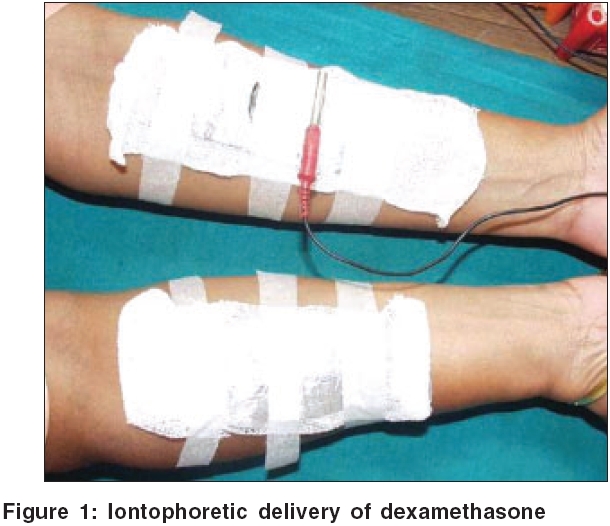
A transparent plastic sheet was used as a template[5] and three apertures (3x3 cm) were cut 2 cm apart. The template was placed on both forearms and with a marker pen, each aperture was outlined. The squares on both forearms were marked 1, 2 and 3, from distal to proximal. Two ml (8 mg) of dexamethasone solution was soaked in a gauze piece and placed on the left forearm. An aluminum foil used as an electrode was placed over the gauze piece and this was connected to the negative electrode since dexamethasone is negatively charged [Figure - 1]. The passive electrode was placed under the feet. Similarly, a dexamethasone soaked gauze piece was placed on the right forearm, but not connected to the iontophoretic machine. Electric current was delivered for 15 minutes and amperage was determined according to the tolerance of the patient. The electrode was removed and both hands wiped with a dry gauze piece. Prick testing with histamine solution was done at the end of 30 min, 1 hour and 2 hours, starting from the last square on both forearms. A drop of 0.1% w/v of histamine solution was placed on the test site. The skin was pricked through the histamine solution with a lancet. The tip of lancet was kept parallel to the skin surface and the skin lifted by tenting the lancet by 45-60° [Figure - 2].
After one minute, the test site was wiped with filter paper to remove the excess histamine solution. The size of wheal was recorded in millimeters after 15 minutes. The mean size of wheal was calculated by measuring the maximum diameter and the orthogonal diameter of the wheal with a transparent scale. Statistical analysis was done using independent t-test. Analysis was two tailed.
Results
The mean standard deviation (SD) of wheal diameter with and without iontophoresis is shown in [Table - 1].
At the end of 30 min, the wheal diameter on the left arm (with IP) was lower than the right one. This difference was statistically significant ( p =0.006). However, at the end of one hour and two hours, there was no statistically significant difference in wheal suppression on the left arm compared to the right one.
Discussion
Iontophoresis has been used to deliver drugs like antivirals for herpes simplex infection,[6] histamine for leg ulcers,[7] local anesthetics,[8] hyaluronidase for scleroderma[9] and lymphedema[10] and sodium salicylate for plantar warts[11] and hyperhidrosis.[12] Methylprednisolone by iontophoresis has been used for aphthous stomatitis and oral lichen planus.[13]
The ability of topical steroids to inhibit a histamine-induced wheal is a simple, safe and easy method to assess their efficacy.[4] Effect of frequency of application of topical steroids[14] and the efficacy of half an hour versus three hour contact of topical steroids have been studied by this method.[5]
We conclude that topical dexamethasone delivered by iontophoresis effectively suppresses the histamine wheal at the end of 30 minutes, but the effect decreases at the end of 1 hour. Since at the end of 30 minutes there was a statistically significant difference in wheal suppression on the left side where iontophoresis was used, we conclude that topical dexamethasone by iontophoresis has the maximum effect at the end of 30 minutes and is more effective than dexamethasone without iontophoresis.
Although steroids are available as topical preparations, their action is limited to the skin and subcutaneous tissue and hence they are used in chronic dermatoses. Delivery of topical steroids by iontophoresis for chronic dermatoses can be time- consuming and cumbersome for patients. Since iontophoresis leads to increased perfusion of deeper tissue, it is recommended for the treatment of deeper structures such as joints and muscles or it can be used instead of intralesional steroid injections. The method may be of practical importance in the treatment of keloids, joint involvement in rheumatoid arthritis and psoriatic arthritis
Further studies are being conducted to compare the relative efficacy of commercially available topical steroids and steroids delivered by iontophoresis.
| 1. |
Kassan DG. Lynch AN, Stiller MJ. Physical enhancement of dermatologic drug delivery. Iontophoresis and phonophoresis. J Am Acad Derm 1996;34:656-66.
[Google Scholar]
|
| 2. |
Crumay MH. Direct iontophoresis and Galvanic surgery. In: Goldsmith H editor. Physical Modalities in Dermatologic Therapy. 1st ed. New York: Springer Verlag; 1978. p. 190-3.
[Google Scholar]
|
| 3. |
Papa CM, Kligman AM. Mechanism of eccrine anhidrosis. J Invest Dermatol 1966;47:1-9.
[Google Scholar]
|
| 4. |
Reddy BS, Singh G. A New model for human bioassay of topical steroids. Br J Dermatol 1976;94:191-3.
[Google Scholar]
|
| 5. |
Rai R, Uppal M, Sharma NK, Srinivas CR, Anil M. Half an hour versus three hour contact of topical steroids. Indian J Dermatol Venereol Leprol 2004;70:214-6.
[Google Scholar]
|
| 6. |
Gangarosa LP, Merchant HW, Park NH, Hill JM. Iontophoretic application of idoxuridine for recurrent herpes labialis: Report of preliminary clinical findings. Methods Find Exp Clin Pharmacol 1979;1:105-9.
[Google Scholar]
|
| 7. |
Abramson DI, Tuck S, Chu LS, Buso E. Physiologic and clinical basis for histamine by ion transfer. Arch Phys Med Rehabil 1967;48:583-91.
[Google Scholar]
|
| 8. |
Gangarosa LP Sr. Iontophoresis for surface local anesthesia. J Am Dent Assoc 1974;88:125-8.
[Google Scholar]
|
| 9. |
Popkin RJ. The use of hyaluronidase by iontophoresis in the treatment of generalized scleroderma. J Invest Dermatol 1951;16:97-102.
[Google Scholar]
|
| 10. |
Schwartz HS. Use of hyaluronidase by iontophoresis in treatment of lymphedema. Arch Intern Med 1955;95:662-8.
[Google Scholar]
|
| 11. |
Gordon NH, Weinstein MV. Sodium salicylate iontophoresis in the treatment of plantar warts (A case report) Phys Ther 1969;49:869-70.
[Google Scholar]
|
| 12. |
Levit F. Treatment of hyperhidrosis by tap water iontophoresis. Cuis 1980;26:192-4.
[Google Scholar]
|
| 13. |
Gangarosa LP Sr. Iontophoresis in dental practive. Chicago: Quintessence Punlishing Co. Inc; 1983. p. 40-52.
[Google Scholar]
|
| 14. |
Sharma N, Srinivas CR, Mathew AC. Effect of frequency of topical corticosteroid application on histamine induced wheal. Int J Dermatol 2005;44:425-7.
[Google Scholar]
|
Fulltext Views
1,854
PDF downloads
862





